The peculiar sensation of hearing a rubber-band-like sound within the ear represents one of the most distinctive and concerning auditory phenomena that patients encounter. This elastic snapping noise, often described as resembling the plucking of a tight elastic band near the eardrum, can range from occasional mild disturbances to persistent, debilitating episodes that significantly impact quality of life. Unlike conventional tinnitus or the familiar crackling sounds associated with pressure changes, rubber-band ear sounds present unique diagnostic challenges due to their complex underlying mechanisms involving multiple anatomical structures within the auditory system.
Medical professionals recognise this symptom as part of a broader spectrum of middle ear myoclonus conditions, where involuntary muscle contractions create distinctive acoustic phenomena. The interconnected nature of the ear’s mechanical components means that disruptions in any single element can manifest as these characteristic elastic sounds, making proper diagnosis essential for effective treatment outcomes.
Anatomical origins of tympanic membrane Rubber-Band sensations
The human ear’s intricate mechanical design creates multiple pathways through which rubber-band sounds can emerge. Understanding these anatomical foundations provides crucial insight into why certain individuals experience these distinctive auditory phenomena whilst others remain unaffected by similar underlying conditions.
Middle ear ossicular chain dysfunction and stapedius muscle spasms
The stapedius muscle, positioned within the middle ear cavity, serves as one of the body’s smallest yet most significant protective mechanisms against acoustic trauma. When this muscle experiences involuntary spasms, it creates rhythmic contractions that directly impact the stapes bone’s position against the oval window. These rapid muscular contractions generate mechanical vibrations that patients often perceive as sharp, elastic snapping sounds.
Stapedius muscle dysfunction frequently develops following exposure to loud noises, viral infections, or as a secondary response to stress-related tension. The muscle’s hyperactive state results in repetitive contractions that occur independently of normal acoustic reflexes, creating the characteristic rubber-band sensation. Research indicates that approximately 15% of individuals experiencing middle ear myoclonus report stapedius-related symptoms as their primary complaint.
Eustachian tube pressure differentials and myringotympanitis effects
Eustachian tube dysfunction creates significant pressure imbalances between the middle ear cavity and the external environment. When these pressure differentials become pronounced, the tympanic membrane experiences abnormal tension states that contribute to elastic sound perception. The membrane’s response to these pressure changes often manifests as sudden snapping sensations, particularly during activities that further alter middle ear pressure.
Chronic myringotympanitis, characterised by persistent inflammation of both the eardrum and middle ear lining, exacerbates these pressure-related phenomena. The inflammatory process increases tissue sensitivity and alters normal membrane compliance, making patients more susceptible to perceiving subtle mechanical changes as prominent rubber-band sounds. Clinical observations suggest that patients with concurrent sinus conditions show increased prevalence of these symptoms.
Tensor tympani syndrome and protective reflex mechanisms
Tensor tympani syndrome represents a distinct condition where the tensor tympani muscle becomes hyperactive, responding inappropriately to normal environmental stimuli. This muscle, responsible for dampening loud sounds by tensing the tympanic membrane, can develop a state of chronic hypervigilance that results in frequent, involuntary contractions.
Patients with tensor tympani syndrome often describe their symptoms as rhythmic clicking or snapping sounds that coincide with specific triggers such as sudden movements, stress, or even anticipation of loud noises. The condition demonstrates a strong correlation with anxiety disorders and hyperacusis, suggesting neurological involvement beyond simple mechanical dysfunction. Treatment approaches typically focus on both muscular relaxation techniques and addressing underlying stress factors.
Malleus and incus displacement contributing to elastic sound perception
The malleus and incus bones form critical components of the ossicular chain, transmitting sound vibrations from the tympanic membrane to the inner ear. Displacement or fixation of these bones can create abnormal mechanical relationships that generate rubber-band-like sounds during head movements or jaw function. Trauma, infection, or congenital abnormalities may cause these bones to lose their normal positioning or mobility.
When ossicular displacement occurs, patients typically experience symptoms that worsen with specific head positions or during activities involving jaw movement. The altered mechanics of sound transmission create intermittent contact between bones or surrounding tissues, producing the characteristic elastic snapping sensation. Diagnostic imaging often reveals subtle positional changes that explain the mechanical basis for these auditory phenomena.
Pathophysiological conditions manifesting as elastic auditory phenomena
Various disease processes can directly or indirectly contribute to rubber-band ear sounds through their effects on middle ear structures, neurological pathways, or vascular components. These conditions often present with additional symptoms that help guide diagnostic evaluation and treatment planning.
Patulous eustachian tube syndrome and autophony symptoms
Patulous eustachian tube syndrome occurs when the normally closed eustachian tube remains abnormally open, allowing continuous air exchange between the middle ear and nasopharynx. This condition creates a unique acoustic environment where patients can hear their own breathing, heartbeat, and voice with unusual clarity—a phenomenon known as autophony.
The persistent opening of the eustachian tube alters normal middle ear mechanics, making the tympanic membrane more responsive to minor pressure fluctuations and internal body sounds. Patients often report that their elastic ear sounds synchronise with breathing patterns or become more prominent during physical exertion.
The condition affects approximately 0.3% of the population, with higher prevalence among individuals who have experienced significant weight loss or hormonal changes.
Otosclerosis-related stapes fixation and conductive hearing loss
Otosclerosis involves abnormal bone growth around the stapes footplate, gradually restricting its mobility within the oval window. This progressive fixation alters the normal mechanical properties of the middle ear system, sometimes creating conditions where residual stapes movement generates unusual acoustic sensations, including rubber-band-like sounds.
As otosclerosis advances, patients may experience intermittent elastic sounds during early stages when the stapes retains partial mobility. These symptoms often coincide with progressive hearing loss and may worsen during periods of hormonal fluctuation. The condition demonstrates genetic predisposition, with approximately 10% of Caucasian populations carrying genes associated with otosclerosis development. Surgical intervention through stapedectomy can effectively address both hearing loss and associated acoustic phenomena in suitable candidates.
Temporal mandibular joint disorders affecting auricular cartilage
Temporomandibular joint dysfunction creates mechanical stress that extends beyond the jaw joint itself, affecting surrounding structures including the external auditory canal and middle ear space. The close anatomical proximity between the TMJ and the ear means that joint inflammation, muscle tension, or structural abnormalities can directly influence auditory perception.
Patients with TMJ disorders frequently report that their ear symptoms, including rubber-band sounds, correlate with jaw movement, chewing, or teeth clenching episodes. The mechanical coupling between jaw function and middle ear pressure creates a pathway through which TMJ dysfunction can manifest as distinctive auditory phenomena. Research indicates that up to 60% of TMJ disorder patients experience some form of auditory symptoms, with elastic sounds representing a significant subset of these complaints.
Meniere’s disease endolymphatic hydrops and tympanic pressure changes
Meniere’s disease involves fluid imbalance within the inner ear’s endolymphatic system, creating pressure fluctuations that can affect middle ear mechanics. During acute episodes or prodromal phases, patients may experience various auditory phenomena, including rubber-band-like sounds that precede or accompany more typical Meniere’s symptoms such as vertigo and hearing fluctuation.
The endolymphatic hydrops characteristic of Meniere’s disease creates dynamic pressure changes that influence the entire auditory system’s mechanical properties. These pressure fluctuations can trigger abnormal middle ear responses, particularly in patients with concurrent eustachian tube dysfunction or middle ear pathology. Clinical evidence suggests that early-stage Meniere’s disease may present primarily with unusual auditory symptoms before classic vertiginous episodes develop.
Neurological factors behind phantom elastic sound perception
The nervous system’s role in generating and perceiving rubber-band ear sounds extends beyond simple mechanical dysfunction, encompassing complex neurological pathways that can create phantom auditory sensations even in the absence of physical middle ear abnormalities.
Trigeminal nerve branch irritation and otic ganglion dysfunction
The trigeminal nerve’s extensive distribution includes branches that innervate structures throughout the ear region. Irritation or inflammation of these neural pathways can generate abnormal sensory signals that the brain interprets as distinctive sounds, including elastic snapping sensations. This neurological mechanism explains why some patients experience rubber-band sounds without identifiable mechanical causes.
Otic ganglion dysfunction represents another neurological pathway through which elastic ear sounds may develop. This parasympathetic ganglion influences middle ear muscle function and vascular control, and its dysfunction can create altered sensory processing that manifests as unusual auditory phenomena. Neurological evaluation becomes particularly important when patients report symptoms that don’t correlate with physical examination findings or imaging studies.
Acoustic neuroma compression effects on cochlear nerve function
Acoustic neuromas, though relatively rare, can create various auditory symptoms through their compressive effects on the eighth cranial nerve. As these benign tumours grow, they may initially cause subtle changes in auditory processing that patients perceive as unusual sounds, including elastic or clicking sensations, before more obvious symptoms like unilateral hearing loss develop.
The progressive nature of acoustic neuroma symptoms means that rubber-band ear sounds may represent early warning signs of tumour presence. These symptoms typically demonstrate unilateral presentation and may worsen gradually over time. Magnetic resonance imaging remains the gold standard for acoustic neuroma detection, particularly when patients present with unexplained unilateral auditory symptoms that don’t respond to conventional treatments.
Temporal lobe epilepsy and auditory hallucination manifestations
Temporal lobe epilepsy can produce complex auditory hallucinations that include mechanical sounds resembling rubber-band snapping or clicking. These seizure-related phenomena differ from peripheral ear conditions in their association with other neurological symptoms and their response to anticonvulsant medications.
Patients experiencing seizure-related auditory phenomena often report that their symptoms occur in distinct episodes, sometimes preceded by aura symptoms or accompanied by altered consciousness states. The auditory hallucinations may include not only rubber-band sounds but also more complex auditory experiences such as music or voices. Electroencephalography and neurological evaluation help distinguish these central causes from peripheral ear disorders.
Tinnitus subtype classification and somatosensory pulsatile variants
Rubber-band ear sounds represent a specific subtype within the broader classification of tinnitus phenomena. Understanding these subtypes helps clinicians develop targeted treatment approaches based on the underlying mechanisms involved.
Somatosensory tinnitus, which includes rubber-band sounds, affects approximately 20% of all tinnitus patients and demonstrates unique characteristics including modulation by jaw movement, neck position, or eye gaze direction.
Pulsatile variants of rubber-band sounds synchronise with heartbeat or respiratory patterns, suggesting vascular involvement in symptom generation. These rhythmic elastic sounds may indicate underlying vascular abnormalities such as arteriovenous malformations or increased intracranial pressure. Detailed history-taking helps distinguish between different tinnitus subtypes and guides appropriate diagnostic evaluation.
Environmental and lifestyle triggers of Rubber-Band ear sounds
External factors and lifestyle choices significantly influence the frequency and intensity of rubber-band ear sounds. Understanding these triggers enables patients to develop effective management strategies whilst helping clinicians identify modifiable risk factors that contribute to symptom development.
Barometric pressure changes represent one of the most commonly reported environmental triggers for elastic ear sounds. Weather fronts, altitude changes, and even indoor pressure variations from heating and cooling systems can precipitate symptoms in susceptible individuals. The mechanism involves middle ear pressure imbalances that stress the tympanic membrane and associated structures, creating conditions conducive to abnormal sound generation. Patients frequently report increased symptom frequency during seasonal weather transitions or when travelling to different elevations.
Stress and anxiety play crucial roles in symptom development through multiple pathways. Psychological tension increases muscle tension throughout the body, including the tiny muscles within the middle ear. This increased muscular tension creates a hypervigilant state where normal acoustic reflexes become overactive, generating inappropriate muscle contractions that patients perceive as rubber-band sounds. Additionally, stress affects sleep quality and immune function, both of which influence overall ear health and symptom susceptibility.
Dietary factors also contribute to symptom patterns, particularly foods that affect vascular function or inflammation levels. Caffeine consumption can increase muscle tension and alter blood flow patterns that influence middle ear mechanics. Similarly, high sodium intake may affect fluid balance throughout the body, including the delicate fluid systems within the ear. Some patients report symptom improvement when following anti-inflammatory dietary approaches that emphasise omega-3 fatty acids and limit processed foods.
Sleep deprivation and irregular sleep patterns create multiple pathways through which rubber-band ear sounds may worsen. Poor sleep affects stress hormone levels, immune function, and neurological processing, all of which influence auditory symptom perception. The position-dependent nature of some ear symptoms means that sleep positioning may also directly affect symptom occurrence, with some patients noting increased symptoms when sleeping on particular sides.
Diagnostic approaches for identifying elastic auditory disturbances
Comprehensive diagnostic evaluation for rubber-band ear sounds requires a systematic approach that encompasses detailed history-taking, physical examination, and appropriate diagnostic testing. The complexity of potential underlying causes necessitates careful consideration of multiple diagnostic pathways to ensure accurate identification of contributing factors.
Initial clinical assessment begins with thorough symptom characterisation, including timing patterns, trigger identification, and associated symptoms. Patients should maintain detailed symptom diaries that document frequency, duration, and circumstances surrounding symptom occurrence. This information helps differentiate between various potential causes and guides subsequent diagnostic testing. The relationship between symptoms and activities such as jaw movement, swallowing, or position changes provides crucial diagnostic clues about underlying mechanisms.
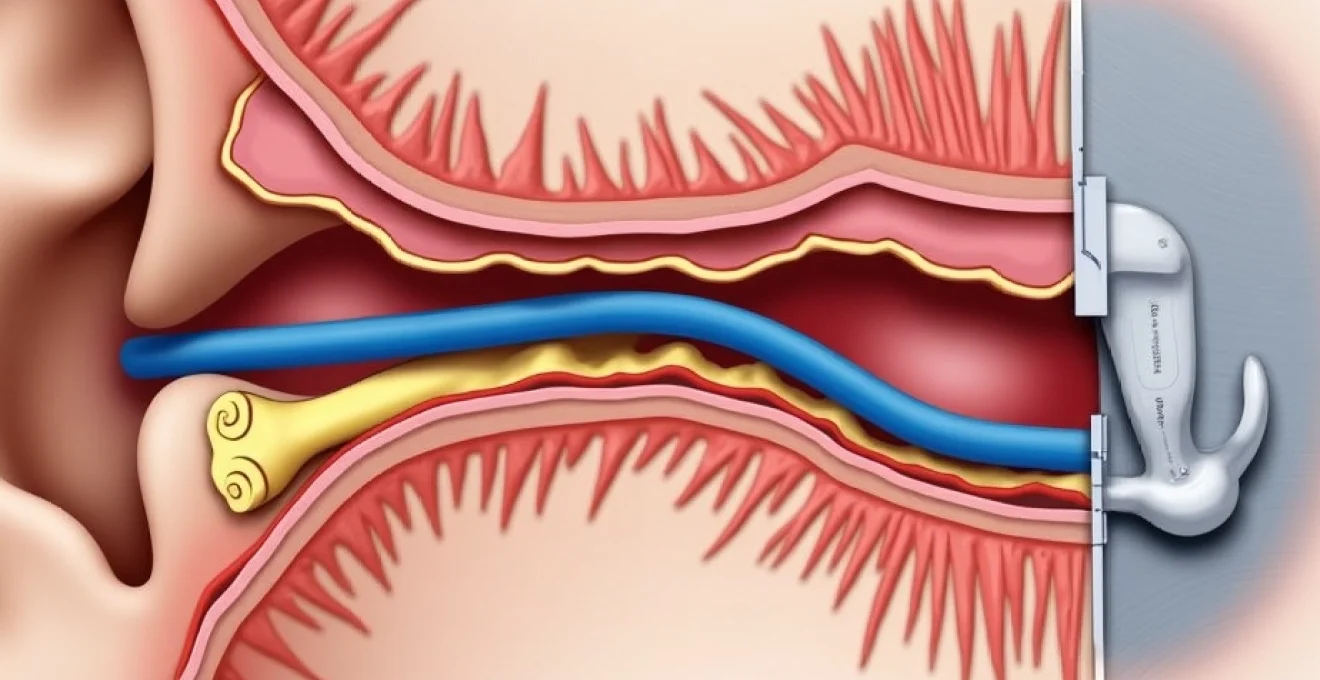
Otoscopic examination forms the foundation of physical assessment, allowing direct visualisation of the tympanic membrane and external auditory canal. Advanced otoscopy techniques, including pneumatic otoscopy and tympanometry, assess middle ear mechanics and eustachian tube function. These tests provide objective measures of middle ear pressure, membrane mobility, and acoustic reflex function that help identify mechanical causes of rubber-band sounds.
Audiometric testing establishes baseline hearing function and identifies any associated hearing loss patterns. Pure tone audiometry, speech audiometry, and impedance testing create a comprehensive picture of auditory system function. Specialised testing such as acoustic reflex decay testing can identify retrocochlear pathology, while otoacoustic emissions testing assesses inner ear function. These objective measures help differentiate between conductive, sensorineural, and mixed hearing loss patterns that may contribute to symptom development.
Advanced imaging studies become necessary when initial evaluation suggests structural abnormalities or when symptoms don’t respond to conservative treatments. High-resolution computed tomography provides detailed visualisation of temporal bone anatomy, including ossicular chain integrity and middle ear inflammation. Magnetic resonance imaging offers superior soft tissue contrast for identifying acoustic neuromas, inflammatory conditions, or vascular abnormalities that may contribute to symptom generation.
| Diagnostic Test | Primary Purpose | Specific Findings |
| Tympanometry | Middle ear mechanics | Pressure, compliance, reflexes |
| Pure tone audiometry | Hearing threshold assessment | Conductive vs sensorineural loss |
| High-resolution CT | Temporal bone anatomy | Ossicular pathology, inflammation |
| MRI with contrast | Soft tissue evaluation | Acoustic neuroma, vascular lesions |
Treatment protocols and management strategies for tympanic Rubber-Band syndrome
Effective management of rubber-band ear sounds requires individualised treatment approaches
that address the specific underlying mechanisms responsible for symptom generation. Understanding the multifaceted nature of these auditory phenomena allows healthcare providers to develop comprehensive treatment plans that target both immediate symptom relief and long-term management strategies.
Conservative management approaches often serve as the initial treatment strategy for patients experiencing rubber-band ear sounds. These non-invasive interventions focus on addressing modifiable factors that contribute to symptom development whilst avoiding potential complications associated with more aggressive treatments. Stress reduction techniques, including mindfulness meditation and progressive muscle relaxation, help address the neurological components of middle ear muscle hyperactivity.
Pharmacological interventions may target specific pathways involved in symptom generation. Muscle relaxants such as baclofen or cyclobenzaprine can reduce middle ear muscle spasms when mechanical causes predominate. Anticonvulsant medications like gabapentin or pregabalin demonstrate efficacy in managing neurologically-mediated auditory symptoms, particularly when patients experience concurrent neuropathic pain or heightened sensory sensitivity. Beta-blockers may benefit patients whose symptoms correlate with anxiety or cardiovascular factors.
Physical therapy approaches incorporate specialised techniques designed to address musculoskeletal contributors to auditory symptoms. Temporomandibular joint therapy helps patients with concurrent jaw dysfunction, whilst cervical spine mobilisation addresses tension patterns that may influence middle ear mechanics. Manual therapy techniques targeting the suboccipital region and upper cervical spine can reduce referred tension that contributes to middle ear muscle hyperactivity. These approaches demonstrate particular benefit when patients report symptom modulation with head or neck positioning changes.
Clinical studies indicate that multimodal treatment approaches achieve success rates of 70-85% in managing rubber-band ear sounds, compared to 40-50% success rates with single-intervention strategies.
Surgical interventions become necessary when conservative measures fail to provide adequate symptom relief or when specific structural abnormalities require correction. Tympanotomy with middle ear exploration allows direct assessment of ossicular chain integrity and identification of mechanical abnormalities contributing to symptom generation. In cases involving stapedius or tensor tympani muscle dysfunction, selective muscle section may provide definitive symptom resolution.
Advanced surgical techniques include balloon dilation of the eustachian tube for patients with persistent dysfunction, whilst patulous eustachian tube repair addresses cases where abnormal tube patency contributes to symptoms. Ossiculoplasty may be required when imaging studies reveal ossicular chain discontinuity or fixation that creates abnormal mechanical relationships within the middle ear space. These procedures require careful patient selection and thorough preoperative evaluation to ensure optimal outcomes.
Psychological support and counselling play crucial roles in comprehensive management, particularly for patients experiencing significant quality of life impacts from persistent symptoms. Cognitive behavioural therapy helps patients develop coping strategies and addresses anxiety or depression that may accompany chronic auditory symptoms. Tinnitus retraining therapy, when adapted for rubber-band ear sounds, can help desensitise patients to their symptoms and reduce their perceived impact on daily functioning.
Long-term monitoring protocols ensure sustained treatment success and early identification of symptom recurrence or progression. Regular audiometric assessments track any changes in hearing function that might indicate evolving underlying conditions. Patient-reported outcome measures provide objective documentation of treatment efficacy and guide adjustments to management strategies. Follow-up imaging may be necessary when symptoms persist despite appropriate treatment or when new symptoms develop that suggest progression of underlying pathology.
Prevention strategies focus on addressing modifiable risk factors that contribute to symptom development or exacerbation. Stress management techniques, proper sleep hygiene, and dietary modifications help maintain optimal middle ear function whilst reducing triggers for muscle hyperactivity. Environmental modifications, including humidity control and allergen avoidance, address external factors that may influence eustachian tube function and middle ear mechanics.
Patient education remains fundamental to successful long-term management, ensuring individuals understand their condition’s underlying mechanisms and can actively participate in treatment decisions. Clear communication about realistic treatment expectations helps prevent frustration when symptoms require prolonged management rather than immediate resolution. Providing patients with resources for symptom tracking and self-management techniques empowers them to take active roles in their care whilst maintaining appropriate medical oversight for ongoing symptom evaluation and treatment optimisation.