Herpes simplex virus infections affecting the buttock crease and perianal regions present unique clinical challenges that often go unrecognised or misdiagnosed. These manifestations of genital herpes, particularly in the intergluteal fold, represent a significant portion of sacral herpes cases that can cause considerable discomfort and confusion for patients. The anatomical location creates an environment conducive to viral reactivation whilst simultaneously complicating both diagnosis and treatment approaches. Understanding the distinctive characteristics of buttock crease herpes outbreaks is essential for healthcare professionals and patients alike, as these infections can mimic various other dermatological conditions and require specialised management strategies.
Clinical identification of gluteal cleft herpes simplex virus lesions
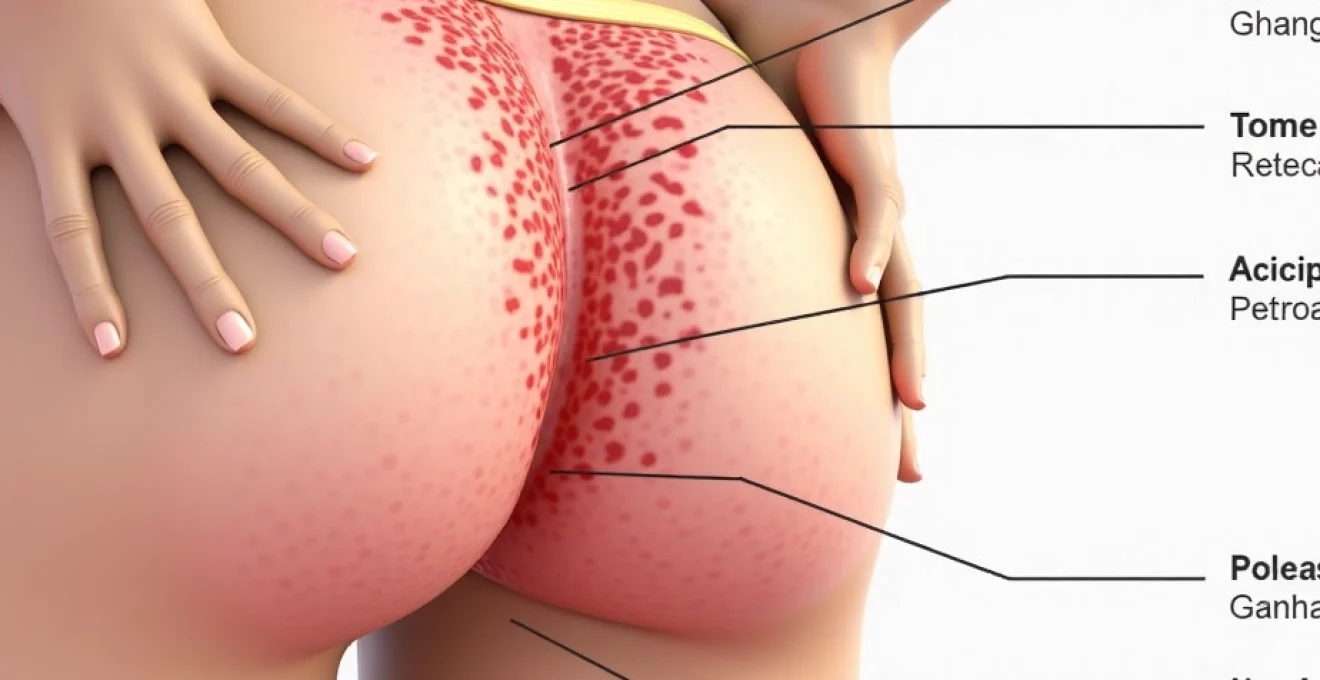
Recognising herpes simplex virus lesions within the gluteal cleft requires careful attention to morphological characteristics and distribution patterns that distinguish these infections from other common conditions affecting the buttock region. The presentation can vary significantly depending on whether the patient is experiencing a primary infection or recurrent episode, with initial outbreaks typically presenting more severe symptoms and extensive lesion distribution.
Primary HSV-1 and HSV-2 vesicular eruptions in intergluteal regions
Primary herpes infections in the buttock crease typically manifest as clusters of small, fluid-filled vesicles that develop over a period of several days. These vesicles, measuring 2-4 millimetres in diameter, appear on an erythematous base and contain clear or slightly turbid fluid. The lesions follow a characteristic pattern of evolution, beginning as small papules that rapidly develop into vesicles before rupturing to form shallow, painful ulcerations with irregular borders.
The distribution of primary lesions often extends beyond the immediate intergluteal fold, potentially involving the lower sacral region, perianal area, and medial aspects of the buttocks. Primary infections typically present with constitutional symptoms including fever, malaise, and regional lymphadenopathy, particularly affecting the inguinal and sacral lymph nodes. The duration of primary episodes can extend from 10 to 21 days, with complete healing occurring without scarring in most cases.
Differential diagnosis from hidradenitis suppurativa and pilonidal cysts
Distinguishing herpes lesions from other conditions affecting the gluteal cleft requires careful consideration of lesion morphology, distribution, and associated symptoms. Hidradenitis suppurativa typically presents with deeper, more inflammatory nodules and abscesses that develop along apocrine gland-bearing areas. The chronic, scarring nature of hidradenitis suppurativa contrasts sharply with the acute, self-limiting course of herpes infections.
Pilonidal cysts and associated infections present as deeper-seated inflammatory lesions, often accompanied by visible pits or openings in the natal cleft. These conditions typically lack the vesicular stage characteristic of herpes and tend to recur in the same anatomical location due to mechanical factors rather than viral reactivation patterns. The pain associated with pilonidal disease is often more constant and pressure-related, whilst herpes-associated discomfort tends to be more acute during active lesion formation.
Dermatoscopic features of perianal herpetic ulcerations
Dermatoscopic examination of perianal herpetic lesions reveals specific features that can aid in diagnosis. Fresh vesicles demonstrate a characteristic peripheral rim of erythema surrounding a central fluid-filled cavity. As lesions progress to the ulcerative stage, dermatoscopy reveals well-demarcated borders with a clean, non-purulent base that distinguishes herpes ulcerations from bacterial infections.
The dermatoscopic appearance of healing herpes lesions shows gradual re-epithelialisation from the periphery inward, with new epithelium appearing pink and slightly raised compared to surrounding normal skin. This pattern of healing helps differentiate herpes from conditions such as aphthous ulceration or traumatic lesions, which may show different healing characteristics.
Laboratory confirmation through PCR testing and tzanck smear analysis
Polymerase chain reaction (PCR) testing represents the gold standard for confirming herpes simplex virus infections in the buttock crease region. PCR testing offers superior sensitivity and specificity compared to viral culture, particularly for lesions that have begun the healing process or in cases where sample quality may be compromised by the anatomical location.
Tzanck smear examination, whilst less sensitive than PCR, can provide rapid preliminary diagnosis by identifying multinucleated giant cells and acantholytic cells characteristic of herpes virus cytopathic effects. The combination of clinical presentation, dermatoscopic features, and laboratory confirmation ensures accurate diagnosis and appropriate treatment initiation. Type-specific serology can provide additional information about the patient’s HSV status and help predict future recurrence patterns.
Anatomical predisposition and viral transmission patterns in buttock crease areas
The anatomical characteristics of the buttock crease create a unique microenvironment that influences both viral transmission and reactivation patterns. Understanding these factors is crucial for developing effective prevention and management strategies for patients experiencing recurrent outbreaks in this region.
Sacrococcygeal and perianal nerve pathway distribution of HSV
Herpes simplex virus establishes latency within the sacral nerve ganglia, specifically the S2-S4 nerve roots that innervate the buttock and perianal regions. This anatomical relationship explains why recurrent herpes outbreaks can manifest anywhere within the sacral dermatome distribution, including the lower buttocks, perianal area, and posterior thigh regions. The nerve pathway distribution determines the precise location where recurrent lesions will appear, often following the same pattern with each episode.
The complex innervation of the gluteal region involves multiple nerve branches, including the posterior femoral cutaneous nerve, inferior cluneal nerves, and branches of the pudendal nerve. This intricate network means that prodromal symptoms such as tingling, burning, or hyperaesthesia may be felt across a broader area than where visible lesions eventually appear.
Occlusive environment and Moisture-Related viral reactivation triggers
The intergluteal fold creates an inherently occlusive environment characterised by increased temperature, humidity, and reduced air circulation. These conditions can serve as triggers for viral reactivation, particularly when combined with other precipitating factors such as friction, stress, or immunosuppression. The moist, warm environment of the buttock crease not only promotes viral reactivation but also potentially prolongs healing times compared to lesions in more exposed areas.
The occlusive nature of the gluteal cleft environment creates ideal conditions for viral persistence and reactivation, making this anatomical location particularly susceptible to recurrent herpes outbreaks.
Mechanical factors such as prolonged sitting, tight clothing, or physical activity that increases friction in the gluteal region can contribute to outbreak frequency. The constant apposition of skin surfaces in the natal cleft creates microtrauma that may facilitate viral reactivation and potentially increase viral shedding duration during active episodes.
Sexual transmission routes leading to gluteal fold manifestations
Herpes infections affecting the buttock crease can result from direct sexual transmission during various forms of intimate contact. Anal-receptive sexual activity represents the most direct route for acquiring genital herpes that subsequently manifests in the perianal and gluteal regions. However, transmission can also occur through skin-to-skin contact during other forms of sexual activity, even when visible lesions are not present on the infected partner.
The viral inoculation site may not always correspond to the location of subsequent recurrent outbreaks due to the extensive nerve pathway distribution. Initial infection may occur at the genital area, with the virus establishing latency in sacral ganglia and later reactivating in the buttock or perianal region. This pattern explains why some patients may experience their first recognised outbreak in the gluteal region despite having been infected through genital contact.
Autoinoculation mechanisms from genital to perirectal sites
Autoinoculation represents another important mechanism by which herpes infections can spread to the buttock crease from existing genital lesions. This process typically occurs during active outbreaks when viral shedding is highest, and can happen through direct contact or via contaminated fingers or objects. Proper hygiene practices during active outbreaks are essential to prevent this form of viral spread.
The risk of autoinoculation is particularly elevated during primary infections when viral shedding is most extensive and patients may be unaware of proper precautionary measures. Healthcare providers should emphasise the importance of hand hygiene and avoiding touching lesions to prevent inadvertent spread to other body areas, including the buttock region.
Pharmacological management of intergluteal herpes outbreaks
Managing herpes outbreaks in the buttock crease requires a comprehensive pharmacological approach that addresses both acute symptom relief and long-term outbreak prevention. The unique anatomical location presents specific challenges for topical medication application and absorption, necessitating tailored treatment strategies.
Topical aciclovir 5% cream application protocols for gluteal lesions
Topical aciclovir cream can provide localised antiviral activity for buttock crease herpes lesions, though its effectiveness is somewhat limited compared to systemic therapy. Proper application technique is crucial for maximising therapeutic benefit in this anatomically challenging region. The cream should be applied in a thin layer to clean, dry lesions every four hours while awake, with particular attention to ensuring adequate coverage of all affected areas.
The occlusive nature of the gluteal environment can actually enhance topical medication absorption, but may also increase the risk of local irritation or secondary bacterial infection. Patients should be advised to gently cleanse the affected area before each application and to use clean hands or applicators to prevent contamination. The application frequency may need adjustment based on individual tolerance and response to treatment.
Systemic antiviral therapy: valaciclovir versus famciclovir efficacy
Systemic antiviral therapy represents the most effective treatment approach for buttock crease herpes outbreaks, with both valaciclovir and famciclovir demonstrating superior efficacy compared to topical treatments. Valaciclovir, administered at doses of 500mg twice daily for episodic treatment or 500mg once daily for suppressive therapy, offers excellent bioavailability and convenient dosing schedules.
Famciclovir provides an alternative option with similar efficacy, typically dosed at 250mg twice daily for episodic treatment. The choice between these medications often depends on patient-specific factors such as renal function, drug interactions, and individual response patterns. Both medications demonstrate excellent safety profiles and can significantly reduce outbreak duration, severity, and viral shedding periods.
Systemic antiviral therapy not only reduces the duration and severity of current outbreaks but also significantly decreases the risk of viral transmission to sexual partners during active episodes.
Adjunctive analgesic management for sacral dermatome pain
Pain management represents a crucial component of treating buttock crease herpes outbreaks, as the rich innervation of this region can result in significant discomfort that extends beyond the visible lesion area. Neuropathic pain characteristics often accompany herpes outbreaks in this location, requiring targeted analgesic approaches that address both inflammatory and neurogenic components.
Topical anaesthetic preparations containing lidocaine or benzocaine can provide localised pain relief, though care must be taken to avoid sensitisation reactions with repeated use. Oral analgesics ranging from simple over-the-counter options like paracetamol and ibuprofen to prescription medications such as gabapentin or pregabalin may be necessary for managing severe neuropathic pain associated with larger or more extensive outbreaks.
Prophylactic suppressive therapy dosing for recurrent episodes
Patients experiencing frequent recurrent outbreaks in the buttock crease may benefit significantly from daily suppressive antiviral therapy. Standard suppressive dosing involves valaciclovir 500mg once daily or famciclovir 250mg twice daily, with treatment duration typically ranging from six months to several years depending on outbreak frequency and patient preference.
The decision to initiate suppressive therapy should consider outbreak frequency, severity, impact on quality of life, and potential for viral transmission. Suppressive therapy can reduce outbreak frequency by 70-80% in most patients and may also decrease asymptomatic viral shedding, thereby reducing transmission risk to sexual partners.
Complications and secondary bacterial infections in buttock crease herpes
Herpes outbreaks in the buttock crease carry an increased risk of complications due to the anatomical location and environmental factors that characterise this region. The warm, moist, and often occluded environment creates conditions that can promote secondary bacterial infections and delay healing processes. Understanding these potential complications is essential for providing comprehensive patient care and preventing more serious sequelae.
Secondary bacterial infection represents the most common complication of buttock crease herpes, occurring in approximately 10-15% of cases. The disrupted skin barrier created by herpetic ulcerations provides an entry point for pathogenic bacteria, including Staphylococcus aureus, Streptococcus pyogenes, and anaerobic organisms commonly found in the perianal region. Signs of bacterial superinfection include increased erythema extending beyond the original lesion borders, purulent discharge, increased pain, and systemic symptoms such as fever or regional lymphadenitis.
The management of secondary bacterial infections requires prompt antibiotic therapy, typically involving oral antibiotics such as flucloxacillin or co-amoxiclav, depending on the suspected organisms and local resistance patterns. Topical antiseptics may provide additional benefit but should be used cautiously to avoid further skin irritation. In severe cases or immunocompromised patients, intravenous antibiotic therapy may be necessary.
Delayed healing represents another significant concern in buttock crease herpes outbreaks. The constant friction and moisture in this region can significantly prolong the healing process, with some lesions taking several weeks longer to resolve compared to lesions in other anatomical locations. Factors contributing to delayed healing include mechanical trauma from sitting or walking, difficulty maintaining adequate hygiene, and the occlusive environment that impedes proper wound healing.
The risk of complications in buttock crease herpes outbreaks is significantly higher than in other anatomical locations, making early recognition and appropriate management crucial for optimal patient outcomes.
Chronic pain syndromes can develop in some patients following severe or recurrent buttock crease herpes outbreaks. Post-herpetic neuralgia, whilst more commonly associated with varicella-zoster virus infections, can occasionally occur with herpes simplex infections, particularly in older patients or those with compromised immune systems. This chronic pain condition can persist for months or even years after the initial outbreak and may require specialised pain management approaches including anticonvulsants, tricyclic antidepressants, or topical capsaicin preparations.
Hygiene protocols and barrier methods for outbreak prevention
Implementing effective hygiene protocols and barrier methods represents a fundamental aspect of preventing recurrent herpes outbreaks in the buttock crease region. These preventive measures not only reduce the likelihood of outbreak occurrence but also minimise the risk of viral transmission and secondary complications when outbreaks do occur.
Daily hygiene practices should emphasise gentle cleansing of the buttock crease area with mild, fragrance-free soap and lukewarm water. Aggressive scrubbing or harsh soaps can irritate the skin and potentially trigger viral reactivation through microtrauma. After cleansing, the area should be thoroughly dried using a clean towel with gentle patting motions rather than vigorous rubbing. Some patients benefit from using a hair dryer on a cool setting to ensure complete drying of the intergluteal fold.
Moisture management plays a crucial role in preventing outbreak recurrence. The use of absorbent powders containing cornstarch or talc can help maintain dryness in the gluteal region, though care should be taken to avoid products containing fragrances or other potential irritants. Antifungal powders may provide additional benefits for patients prone to concurrent fungal infections in this region.
Clothing choices significantly impact the microenvironment of the
buttock crease region. Loose-fitting cotton underwear and breathable fabrics help reduce friction and allow better air circulation, whilst tight synthetic materials can create an occlusive environment that promotes viral reactivation. During periods of increased physical activity or warm weather, changing underwear more frequently may be necessary to maintain optimal hygiene.
Barrier methods during sexual activity represent a critical component of prevention strategies, particularly for individuals with recurrent buttock crease herpes outbreaks. Latex or polyurethane condoms provide effective protection during anal intercourse, though their protective effect may be limited if lesions extend beyond the covered area. Dental dams offer additional protection during oral-anal contact, whilst female condoms can provide broader coverage for various forms of intimate contact involving the buttock and perianal regions.
Personal hygiene items should be strictly personal and never shared between partners or household members. This includes towels, washcloths, underwear, and any topical medications or ointments used during outbreaks. Separate laundry handling may be advisable during active outbreaks, with affected clothing and linens washed in hot water and thoroughly dried to eliminate any residual viral particles.
Environmental modifications within the home can support outbreak prevention efforts. Maintaining appropriate humidity levels, ensuring adequate ventilation in bathrooms, and using antimicrobial cleaning products on toilet seats and other surfaces that may come into contact with the affected area can reduce the overall viral load in the environment. Regular replacement of personal hygiene items such as loofahs, razors, and washcloths during and after outbreaks prevents reinfection from contaminated materials.
The combination of proper hygiene protocols, appropriate clothing choices, and consistent barrier method use can reduce the frequency of buttock crease herpes outbreaks by up to 60% in compliant patients.
Stress management techniques play an underappreciated role in outbreak prevention, as psychological stress represents one of the most common triggers for herpes reactivation. Regular exercise, adequate sleep, and stress reduction techniques such as meditation or yoga can help maintain immune system function and reduce outbreak frequency. Patients should be counseled about the connection between stress and viral reactivation, with emphasis on developing personalised stress management strategies.
Dietary considerations may also influence outbreak patterns, though the evidence remains largely anecdotal. Some patients report reduced outbreak frequency when avoiding foods high in arginine (such as nuts, chocolate, and seeds) whilst increasing lysine-rich foods (dairy products, fish, and certain vegetables). Maintaining adequate nutrition and hydration supports overall immune function and may contribute to reduced viral reactivation rates.
Partner communication and education represent essential elements of comprehensive prevention strategies. Sexual partners should be informed about the diagnosis and educated about transmission risks, even during asymptomatic periods. Regular STI screening for both partners helps ensure early detection and treatment of any co-infections that might compromise immune function or increase herpes reactivation risk.
The implementation of these hygiene protocols and barrier methods requires consistent application and ongoing adjustment based on individual response patterns. Patients should work closely with their healthcare providers to develop personalised prevention strategies that take into account their specific risk factors, lifestyle considerations, and outbreak patterns. Regular follow-up appointments allow for assessment of prevention strategy effectiveness and modification of approaches as needed to optimise long-term outbreak management and quality of life.