Experiencing dizziness following earwax removal is a common concern that affects many patients, yet understanding the duration and underlying mechanisms remains crucial for managing expectations and ensuring proper care. The vestibular system’s intricate connection to the ear canal means that even routine cerumen extraction procedures can temporarily disrupt balance, leading to sensations ranging from mild lightheadedness to more pronounced vertigo. Professional healthcare providers recognise that whilst dizziness after earwax removal is typically temporary, the duration can vary significantly based on the removal method employed, individual patient factors, and the extent of the original wax impaction.
The complexity of post-removal dizziness stems from the delicate relationship between the external auditory canal and the inner ear’s balance mechanisms. When cerumen becomes impacted, it can create pressure changes and mechanical disturbances that affect not only hearing but also equilibrium. The removal process itself, whether through microsuction, irrigation, or manual extraction, can introduce additional factors that temporarily influence vestibular function, making it essential for patients to understand what constitutes normal recovery patterns versus symptoms requiring further medical attention.
Cerumen impaction and Post-Removal vestibular disturbances
The relationship between earwax buildup and subsequent dizziness following removal involves complex physiological mechanisms that extend beyond simple mechanical obstruction. When cerumen accumulates to the point of impaction, it creates a cascade of pressure changes within the ear canal that can affect the delicate structures responsible for balance and spatial orientation. This impaction doesn’t merely block sound transmission; it can also influence the pressure dynamics within the middle ear space, potentially affecting the vestibular organs located in the inner ear.
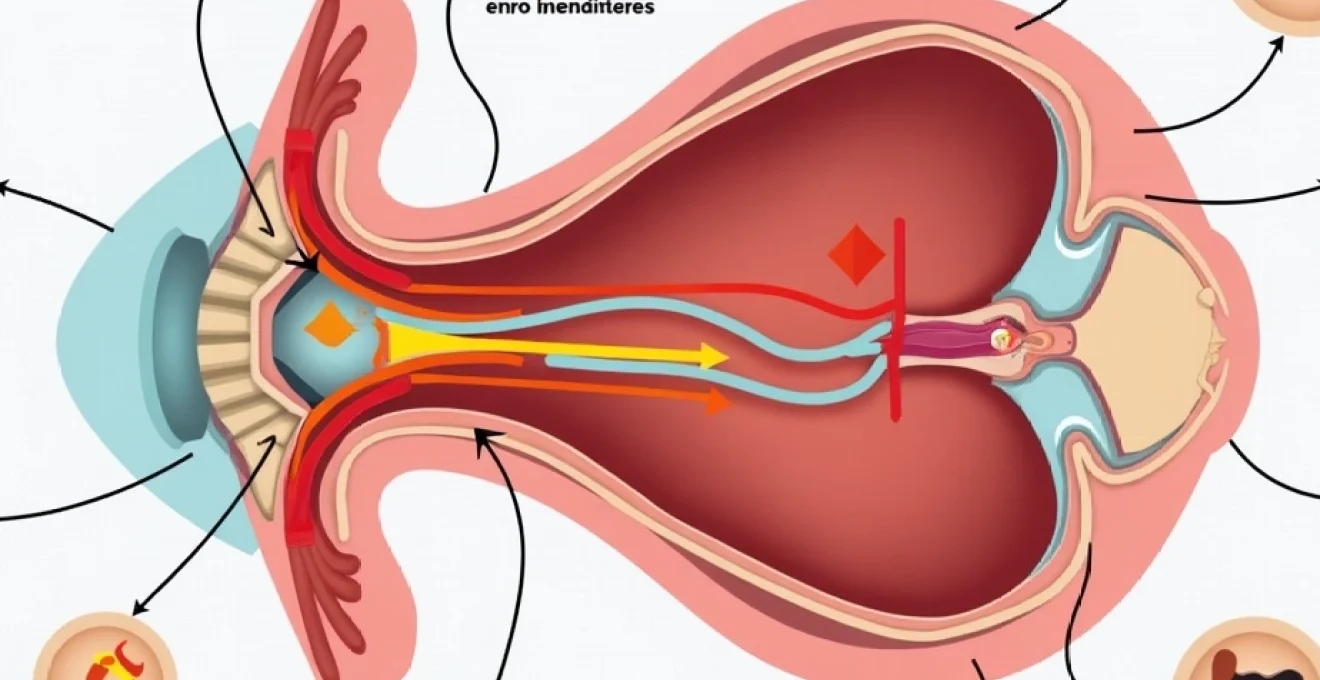
Understanding the anatomical connections between the external ear canal and the vestibular system is crucial for comprehending why dizziness occurs after earwax removal, even in routine procedures performed by experienced professionals.
Anatomy of the external auditory canal and vestibular system connection
The external auditory canal’s proximity to the vestibular apparatus creates a direct pathway through which mechanical disturbances can influence balance function. The ear canal, measuring approximately 24-26mm in length, follows an S-shaped curve that terminates at the tympanic membrane. This membrane serves as a crucial barrier between the external environment and the delicate structures of the middle and inner ear. When cerumen impaction occurs, particularly in the medial third of the canal near the tympanic membrane, the resulting pressure can create mechanical stress on this vital structure.
The vestibular system, housed within the temporal bone’s labyrinthine structure, consists of three semicircular canals, the utricle, and the saccule. These organs detect head movement and gravitational forces through specialised hair cells suspended in endolymph fluid. The close anatomical relationship means that any procedure affecting pressure within the ear canal can potentially influence endolymph dynamics, leading to temporary vestibular disturbances. This connection explains why patients often experience dizziness not only during the removal procedure but also for varying periods afterwards.
Mechanical pressure effects on the tympanic membrane
Impacted cerumen can exert considerable mechanical pressure on the tympanic membrane, creating a state of chronic stress on this delicate structure. The tympanic membrane’s normal position and mobility are essential for proper middle ear function and pressure equalisation. When cerumen presses against this membrane, it can create abnormal pressure gradients that extend into the middle ear space through the Eustachian tube connection. This mechanical pressure doesn’t simply resolve immediately upon wax removal; the tympanic membrane requires time to return to its normal position and function.
The sudden relief of pressure following cerumen extraction can create a temporary imbalance in the pressure dynamics between the external, middle, and inner ear compartments. This pressure differential can stimulate the vestibular organs inappropriately, leading to sensations of dizziness or unsteadiness. The duration of these effects typically correlates with the degree of initial impaction and the length of time the cerumen had been pressing against the tympanic membrane before removal.
Caloric stimulation during microsuction and irrigation procedures
One of the most significant factors contributing to post-removal dizziness involves the inadvertent caloric stimulation that can occur during various earwax removal procedures. The vestibular system is exquisitely sensitive to temperature changes within the ear canal, a principle utilised diagnostically in caloric testing for vestibular function assessment. During earwax removal, particularly with irrigation methods, temperature variations can create convection currents within the ear canal that stimulate the horizontal semicircular canal.
Microsuction procedures can also induce temperature changes through the cooling effect of the suction process itself. As air is drawn through the suction device, it can create a cooling sensation within the ear canal that may be sufficient to stimulate vestibular responses. This caloric effect typically produces a brief episode of nystagmus and accompanying dizziness that can persist for several minutes to hours after the procedure. Understanding this mechanism helps explain why even the most carefully performed procedures can result in temporary vestibular symptoms.
Endolymph displacement following cerumen extraction
The removal of significant cerumen impaction can create subtle but important changes in the fluid dynamics within the inner ear. The endolymph, a potassium-rich fluid that fills the membranous labyrinth, plays a crucial role in vestibular function. Any disturbance that affects the normal pressure relationships within the temporal bone can potentially influence endolymph movement and composition. The sudden change in external ear pressure following wax removal can create transient alterations in endolymphatic pressure through the complex interconnections of the ear’s fluid-filled spaces.
These pressure changes can stimulate the vestibular hair cells inappropriately, creating sensations of movement or imbalance when none actually exists. The restoration of normal endolymphatic pressure and flow patterns typically occurs within hours to days, depending on individual factors such as Eustachian tube function and overall inner ear health. Patients with pre-existing vestibular sensitivities or inner ear conditions may experience more prolonged symptoms as their systems take longer to readjust to the new pressure environment.
Professional earwax removal methods and associated dizziness duration
Different professional earwax removal techniques carry varying risks and durations of post-procedural dizziness, with each method presenting unique mechanisms that can influence vestibular function. The choice of removal technique often depends on the nature and extent of cerumen impaction, patient factors, and practitioner preference. Understanding how each method affects the delicate balance system helps predict recovery timelines and manage patient expectations effectively.
Modern ear care practices have evolved to minimise vestibular disturbances whilst maximising removal efficiency and safety. However, even the most advanced techniques cannot completely eliminate the possibility of temporary dizziness, as the fundamental anatomy and physiology of the ear make some degree of vestibular stimulation inevitable during cerumen extraction. The key lies in understanding which methods pose the greatest risk and implementing strategies to minimise their impact on patient comfort and recovery time.
Microsuction technique recovery timeline and vestibular impact
Microsuction represents the gold standard for professional earwax removal due to its precision and reduced risk of complications. This technique utilises a microscope for visualisation and a gentle suction device to remove cerumen without introducing fluids into the ear canal. Despite its advantages, microsuction can still produce temporary dizziness through several mechanisms, including the cooling effect of air movement and potential mechanical stimulation of the ear canal walls.
The typical recovery timeline following microsuction shows that most patients experience any dizziness for no more than 30 minutes to 2 hours post-procedure. The vestibular disturbance associated with microsuction tends to be milder and shorter in duration compared to irrigation methods. This reduced impact stems from the absence of temperature-variable fluids and the controlled nature of the suction pressure. However, patients with particularly sensitive vestibular systems or those who had extensive impaction may experience symptoms for up to 24 hours.
Individual factors significantly influence recovery time, with older patients or those with pre-existing balance disorders potentially requiring longer periods for complete symptom resolution. The precision of microsuction allows practitioners to avoid excessive manipulation of the ear canal, which helps minimise the duration and severity of post-procedural dizziness. Most patients report that any initial lightheadedness or unsteadiness resolves completely within the first few hours following treatment.
Water irrigation Temperature-Related vertigo following otex softening
Water irrigation methods, particularly when preceded by wax-softening agents, present the highest risk for post-procedural dizziness due to the inevitable caloric stimulation that occurs when water at body temperature or slightly warmer is introduced into the ear canal. The irrigation process typically involves directing a controlled stream of warm water into the ear canal to flush out softened cerumen, but this procedure can inadvertently create strong vestibular responses even when performed correctly.
Following irrigation procedures, patients commonly experience dizziness lasting anywhere from 15 minutes to 6 hours, with the average duration being approximately 2-3 hours. The intensity and duration of symptoms often correlate with the temperature differential between the irrigation fluid and the patient’s core body temperature. Even slight deviations from the optimal temperature range of 37°C can produce significant vestibular stimulation, leading to sensations of spinning, unsteadiness, or general disorientation.
The use of wax-softening preparations such as Otex prior to irrigation can actually contribute to prolonged dizziness recovery times. These preparations can alter the normal protective properties of cerumen and may create additional sensitivity within the ear canal. Patients who have used softening agents for several days before professional removal often report more intense and longer-lasting vestibular symptoms, sometimes extending recovery time to 8-12 hours in sensitive individuals.
Manual removal with jobson horne probe and immediate disorientation
Manual cerumen removal using specialised instruments such as the Jobson Horne probe represents a traditional yet effective method for addressing stubborn or adherent wax deposits. This technique requires considerable skill and experience, as the practitioner must navigate the ear canal’s anatomy whilst maintaining direct contact with the cerumen. The mechanical nature of this removal method can create immediate vestibular stimulation through direct contact with the ear canal walls and potential vibration transmission to the inner ear structures.
The dizziness associated with manual removal typically manifests immediately during or shortly after the procedure, often presenting as a brief but intense sensation of disorientation or imbalance. This immediate response usually resolves within 30-60 minutes, though some patients may experience residual unsteadiness for up to 4 hours. The direct mechanical stimulation inherent in this technique can trigger proprioceptive responses that temporarily confuse the brain’s spatial orientation centres.
Recovery from manual removal-induced dizziness tends to follow a predictable pattern, with the most intense symptoms occurring within the first 15-30 minutes post-procedure. The precision required for safe manual removal means that experienced practitioners can minimise unnecessary manipulation of sensitive canal areas, thereby reducing both the intensity and duration of vestibular symptoms. Patients typically report a rapid improvement in symptoms once the initial disorientation passes, with complete resolution occurring more quickly than with irrigation methods.
Endoscopic wax removal and Post-Procedural balance restoration
Endoscopic earwax removal represents one of the most advanced techniques available, utilising high-definition visualisation to guide precise cerumen extraction with minimal tissue contact. This method combines the advantages of excellent visualisation with reduced mechanical stimulation of the ear canal, theoretically resulting in lower rates of post-procedural dizziness. The endoscopic approach allows practitioners to identify and avoid areas of particular sensitivity whilst ensuring complete wax removal.
Post-endoscopic removal dizziness, when it occurs, typically presents as mild lightheadedness lasting 15-45 minutes. The superior visualisation provided by endoscopic equipment enables practitioners to work more efficiently and with less manipulation of the ear canal walls, directly correlating with reduced vestibular stimulation. This technique particularly benefits patients with narrow or tortuous ear canals, where traditional methods might require more extensive manipulation to achieve complete removal.
The balance restoration process following endoscopic removal tends to be smoother and more predictable than with other methods. The reduced mechanical trauma to the ear canal means that normal vestibular function typically returns within 1-2 hours of the procedure. Patients often report that any initial unsteadiness resolves progressively, with significant improvement noted within the first 30 minutes and complete resolution achieved well before the end of the first post-procedural hour.
Physiological recovery patterns after cerumen extraction
The physiological recovery process following earwax removal follows predictable patterns that reflect the complex interplay between mechanical, thermal, and pressure-related factors affecting the vestibular system. Understanding these recovery patterns helps both patients and healthcare providers distinguish between normal post-procedural effects and symptoms that might indicate complications requiring further attention. The human vestibular system demonstrates remarkable adaptability and resilience, typically restoring normal function within hours of cerumen extraction procedures.
Recovery patterns can be categorised into immediate, short-term, and extended phases, each characterised by distinct physiological processes and symptom presentations. The immediate phase, occurring within the first 30 minutes post-procedure, involves the resolution of acute vestibular stimulation and the restoration of normal pressure gradients within the ear. Short-term recovery, spanning 30 minutes to 6 hours, encompasses the normalisation of endolymphatic pressure and the resolution of any residual caloric effects. Extended recovery, though rare, can occur in sensitive individuals and may last up to 24-48 hours in exceptional circumstances.
The vestibular compensation mechanisms that govern recovery involve multiple levels of the nervous system, from the peripheral vestibular organs through the brainstem vestibular nuclei to the cortical centres responsible for spatial orientation. This multi-level process ensures that even when temporary disruption occurs, the brain can quickly adapt and restore normal balance function. Individual variations in compensation speed explain why some patients recover within minutes whilst others may require several hours to feel completely normal.
Factors influencing recovery speed include age, overall health status, pre-existing vestibular conditions, and individual sensitivity to pressure changes. Younger patients typically demonstrate faster recovery times due to more robust vestibular compensation mechanisms, whilst older adults may require extended periods for complete symptom resolution. The presence of concurrent medical conditions such as Ménière’s disease, benign paroxysmal positional vertigo, or middle ear pathology can significantly extend recovery times and may require additional management strategies.
| Recovery Phase | Duration | Primary Symptoms | Physiological Process |
|---|---|---|---|
| Immediate | 0-30 minutes | Acute dizziness, disorientation | Pressure equalisation, acute vestibular stimulation resolution |
| Short-term | 30 minutes-6 hours | Mild unsteadiness, residual lightheadedness | Endolymphatic pressure normalisation, caloric effect resolution |
| Extended | 6-48 hours | Intermittent imbalance, positional sensitivity | Complete vestibular compensation, tissue healing |
Risk factors influencing Post-Removal dizziness severity
Several patient-specific and procedural factors significantly influence both the likelihood and severity of dizziness following earwax removal. Understanding these risk factors enables healthcare providers to better prepare patients for the procedure and implement appropriate precautionary measures. Age represents one of the most significant risk factors, with patients over 65 years demonstrating increased susceptibility to post-procedural vestibular disturbances due to age-related changes in inner ear function and slower compensation mechanisms.
Pre-existing vestibular disorders substantially increase the risk of prolonged or severe dizziness following cerumen extraction. Conditions such as benign paroxysmal positional vertigo, vestibular neuritis, or Ménière’s disease can predispose patients to more intense and longer-lasting symptoms. The compromised vestibular system in these patients struggles to compensate for the additional disruption caused by the removal procedure, often resulting in symptoms that persist well beyond the typical recovery timeframe.
The degree and duration of cerumen impaction directly correlate with post-removal dizziness severity. Patients with long-standing, complete canal occlusion often experience more pronounced symptoms due to the significant pressure changes that occur when the blockage is removed. The tympanic membrane and middle ear structures require time to readjust to normal pressure conditions, and this adjustment period can manifest as persistent dizziness or unsteadiness.
Medication use can significantly influence vestibular sensitivity and recovery patterns. Patients taking ototoxic medications, certain antibiotics
, antidepressants, or blood pressure medications may experience heightened sensitivity to vestibular disturbances. These medications can affect inner ear function or alter the body’s ability to compensate for balance disruptions, potentially extending recovery times significantly.
Individual anatomical variations also play a crucial role in determining dizziness severity. Patients with narrow ear canals, unusual canal curvature, or previous ear surgery may be more susceptible to procedural complications that increase vestibular symptoms. The proximity of surgical sites or scar tissue to vestibular structures can create additional sensitivity that manifests as prolonged dizziness following routine procedures.
Anxiety and stress levels at the time of the procedure can substantially amplify both the perception and actual severity of post-removal dizziness. The psychological component of balance disorders means that patients who are particularly anxious about the procedure may experience more intense symptoms and slower recovery. This psychosomatic element often requires additional reassurance and support to facilitate optimal recovery outcomes.
Clinical assessment of persistent vertigo following wax removal
When dizziness persists beyond the expected recovery timeframe following earwax removal, comprehensive clinical assessment becomes essential to differentiate between normal recovery variations and pathological conditions requiring intervention. The evaluation process must systematically exclude complications such as tympanic membrane perforation, inner ear injury, or the unmasking of pre-existing vestibular disorders that may have been previously compensated or undiagnosed.
The clinical assessment begins with a detailed history focusing on symptom character, timing, and associated features. Practitioners must distinguish between true vertigo, characterised by a spinning sensation, and other forms of dizziness such as presyncope or disequilibrium. The temporal relationship between the removal procedure and symptom onset provides crucial diagnostic information, as does the pattern of symptom evolution over time.
Physical examination should encompass both otological and neurological components, with particular attention to vestibular function testing. The presence of spontaneous nystagmus, gait instability, or positive Romberg testing may indicate significant vestibular dysfunction requiring further investigation. Otoscopic examination must confirm successful cerumen removal whilst excluding procedural complications such as canal wall injury or residual debris.
Dix-hallpike manoeuvre for BPPV differential diagnosis
The Dix-Hallpike manoeuvre represents a critical diagnostic tool for distinguishing between post-procedural vestibular disturbance and benign paroxysmal positional vertigo that may have been precipitated or unmasked by the earwax removal process. This diagnostic manoeuvre involves rapidly moving the patient from a sitting to a supine position with the head turned 45 degrees and extended below the horizontal plane, effectively stimulating the posterior semicircular canal.
Positive Dix-Hallpike testing in the context of recent earwax removal may indicate that the procedure has displaced otoconia within the semicircular canals, creating secondary BPPV. This complication, whilst uncommon, can occur when mechanical vibrations or pressure changes during removal disturb the delicate calcium carbonate crystals normally situated within the utricle. The resulting vertigo typically presents with characteristic rotatory nystagmus and can persist for days or weeks without appropriate treatment.
The timing and characteristics of nystagmus during Dix-Hallpike testing provide valuable diagnostic information. Classic BPPV-related nystagmus demonstrates a brief latency period followed by rotatory movements that fatigue with repetition. In contrast, central vestibular disorders may produce atypical nystagmus patterns that persist without fatigue, indicating more serious underlying pathology requiring urgent neurological consultation.
Audiometry testing for conductive hearing loss resolution
Comprehensive audiometric evaluation following earwax removal serves multiple diagnostic purposes, confirming successful restoration of hearing whilst identifying potential complications that may contribute to persistent vestibular symptoms. Pure tone audiometry should demonstrate resolution of the conductive hearing loss typically associated with cerumen impaction, with air-bone gaps returning to normal values following successful removal.
Failure to achieve expected hearing improvement may indicate incomplete wax removal, procedural complications, or the presence of additional pathology that was previously masked by the cerumen blockage. Persistent conductive hearing loss could suggest tympanic membrane perforation, ossicular chain disruption, or middle ear effusion secondary to the removal procedure. These complications often present with accompanying vestibular symptoms due to the interconnected nature of hearing and balance systems.
Tympanometry provides additional objective information about middle ear function and can identify pressure abnormalities or membrane mobility issues that might contribute to ongoing dizziness. Type B tympanograms following removal may indicate middle ear effusion or membrane perforation, whilst abnormal acoustic reflex patterns could suggest ossicular chain disruption or facial nerve involvement.
Vestibular function assessment using head impulse testing
The head impulse test offers a rapid, bedside assessment of vestibular function that can identify unilateral vestibular weakness potentially related to removal-associated complications. This test involves applying brief, rapid head movements whilst observing for compensatory saccades that indicate impaired vestibular-ocular reflex function. Abnormal head impulse responses following earwax removal may suggest inner ear injury or exacerbation of pre-existing vestibular pathology.
Video head impulse testing, when available, provides quantitative assessment of vestibular function across all six semicircular canals. This advanced testing can detect subtle vestibular deficits that might not be apparent on clinical examination alone. The ability to identify specific canal dysfunction helps localise pathology and guides appropriate treatment strategies for patients with persistent post-removal symptoms.
The interpretation of vestibular function testing must consider baseline function and age-related changes in vestibular performance. Older patients naturally demonstrate reduced vestibular function, making it essential to distinguish between normal age-related decline and pathological changes related to the removal procedure. Serial testing may be necessary to document recovery patterns and guide ongoing management decisions.
Management strategies for extended Post-Procedural disorientation
When dizziness persists beyond the typical recovery timeframe following earwax removal, implementing targeted management strategies becomes essential for patient comfort and optimal outcomes. The approach to extended post-procedural disorientation must address both symptomatic relief and underlying physiological disturbances whilst monitoring for potential complications requiring medical intervention.
Initial management focuses on vestibular rehabilitation exercises designed to promote central compensation for any residual peripheral vestibular dysfunction. These exercises include progressive head movements, balance training, and habituation protocols that encourage the brain’s natural adaptation mechanisms. The intensity and duration of rehabilitation protocols should be tailored to individual patient tolerance and symptom severity.
Pharmacological intervention may be appropriate in cases of severe or persistent symptoms, though medications should be used judiciously to avoid interfering with natural vestibular compensation processes. Short-term use of vestibular suppressants such as prochlorperazine or betahistine can provide symptomatic relief whilst allowing the underlying recovery processes to continue. However, prolonged use of these medications may actually delay compensation and should be avoided except in exceptional circumstances.
Patient education plays a crucial role in managing extended post-procedural symptoms, helping individuals understand normal recovery patterns whilst providing realistic expectations for symptom resolution. Clear communication about warning signs requiring immediate medical attention empowers patients to participate actively in their recovery whilst seeking appropriate care when necessary. This educational component should emphasise the temporary nature of most post-removal symptoms and provide practical strategies for managing daily activities during the recovery period.
Environmental modifications and safety precautions become particularly important for patients experiencing extended dizziness following earwax removal. Simple measures such as ensuring adequate lighting, removing trip hazards, and using mobility aids when necessary can prevent falls and injuries during the recovery period. Patients should be advised to avoid driving or operating machinery until symptoms resolve completely, prioritising safety over convenience during the healing process.
Follow-up scheduling should be individualised based on symptom severity and patient risk factors, with more frequent monitoring for high-risk patients or those with concerning symptomatology. Regular assessment allows for early identification of complications whilst providing ongoing reassurance and support throughout the recovery process. The combination of appropriate medical management, patient education, and careful monitoring typically results in successful resolution of even extended post-procedural vestibular symptoms.