Experiencing bleeding or spotting after a cervical screening examination is one of the most common concerns women face following their routine gynaecological appointments. This physiological response occurs in approximately 15-20% of patients undergoing Pap smear procedures, according to recent clinical data from major women’s health organisations. The cervix, being a highly vascularised structure with delicate epithelial tissue, naturally responds to the mechanical manipulation required during cell collection with varying degrees of haemorrhage.
Understanding the distinction between normal post-procedural bleeding and concerning haemorrhage patterns is crucial for both patients and healthcare providers. Most bleeding episodes following cervical screening resolve spontaneously within 24-48 hours , representing a benign response to the sampling technique rather than an indication of underlying pathology. However, recognising when bleeding warrants immediate medical attention can prevent potential complications and provide reassurance during what can be an anxiety-provoking experience for many women.
Understanding normal cervical cell collection procedures and expected outcomes
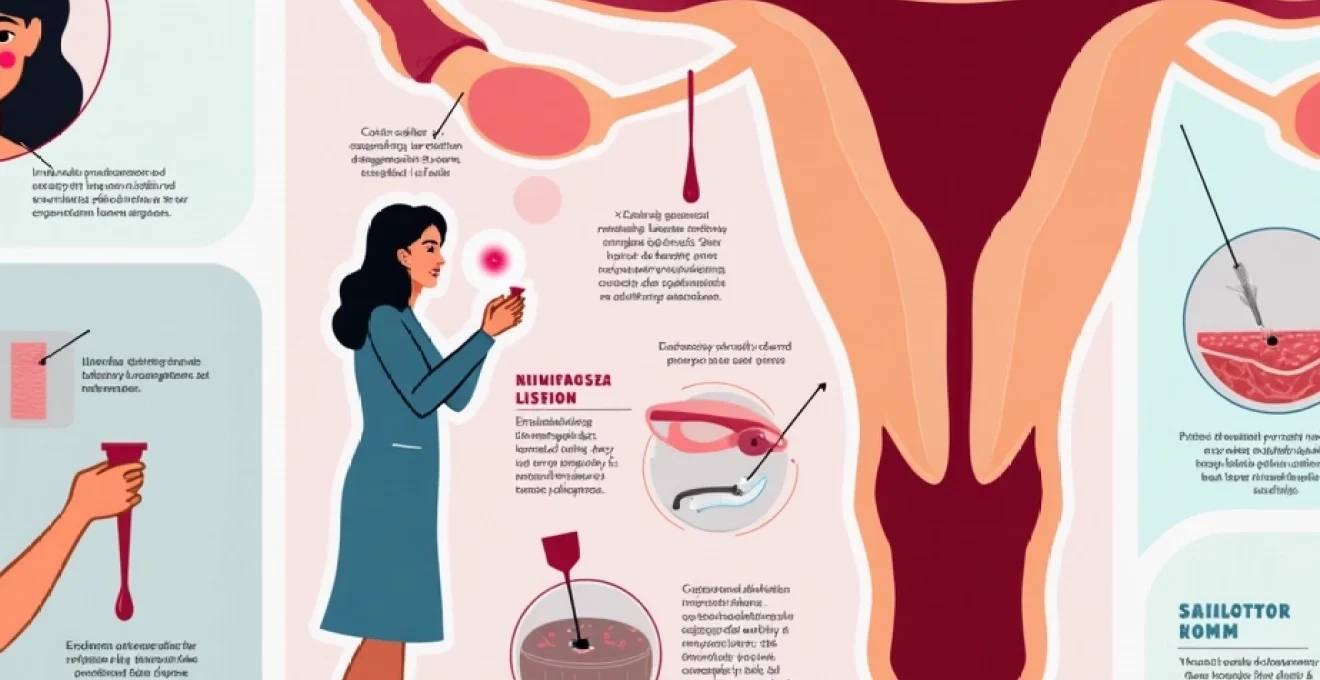
Modern cervical screening programmes employ sophisticated methodologies designed to maximise cellular yield whilst minimising patient discomfort and tissue trauma. The transformation zone, where squamous and glandular epithelia meet, represents the primary target area for specimen collection due to its heightened susceptibility to neoplastic changes. This anatomical region requires careful sampling to ensure adequate representation of both cell types in the cytological preparation.
Liquid-based cytology techniques and endocervical brush methodology
Contemporary liquid-based cytology has revolutionised cervical screening by improving specimen adequacy rates and reducing the need for repeat examinations. The endocervical brush, typically featuring synthetic bristles arranged in a cylindrical configuration, must be inserted into the cervical canal to a depth of approximately 1.5-2 centimetres. This insertion depth ensures adequate sampling of the endocervical columnar epithelium whilst avoiding excessive trauma to the internal os.
The rotational movement required for optimal cell harvest—typically five complete turns in a clockwise direction—creates controlled microabrasions along the cervical canal surface. These microscopic disruptions to the epithelial integrity are necessary for cellular exfoliation but inevitably result in minor capillary bleeding in approximately one-third of patients. The bleeding tendency correlates directly with the firmness of brush application and the number of rotational movements performed .
Cytobrush insertion depth and transformation zone sampling
Optimal cytobrush positioning requires precise anatomical awareness, particularly regarding the location of the squamocolumnar junction. In reproductive-age women, this junction typically lies at or near the external cervical os, whilst in postmenopausal women, it may retreat several millimetres into the endocervical canal. The sampling technique must account for these age-related anatomical variations to ensure adequate transformation zone representation.
Excessive insertion depth can traumatise the delicate endocervical mucosa, leading to increased bleeding propensity and patient discomfort. Conversely, insufficient penetration may result in inadequate glandular cell sampling, necessitating repeat examination. The optimal technique involves gentle insertion until slight resistance is encountered, followed by the standardised rotational movement pattern.
Spatula selection for ectocervical cell harvesting
Ectocervical sampling employs spatulas designed to conform to the cervical anatomy whilst providing adequate surface contact for cellular collection. Modern spatulas feature rounded edges and graduated flexibility to minimise epithelial trauma whilst maintaining effective cell harvest rates. The selection of appropriate spatula size depends upon cervical morphology, with nulliparous women typically requiring smaller implements than multiparous patients.
The sampling motion involves a complete 360-degree sweep around the cervical circumference, applying consistent gentle pressure throughout the rotation. This technique ensures comprehensive ectocervical coverage whilst distributing mechanical stress across the entire transformation zone periphery. Proper spatula positioning and movement significantly influence both specimen adequacy and post-procedural bleeding patterns .
Post-procedural cervical epithelium response patterns
Following successful cell collection, the cervical epithelium initiates immediate healing responses characterised by increased vascular permeability and inflammatory mediator release. These physiological changes typically manifest as transient spotting or light bleeding, beginning within minutes of the examination and persisting for 12-72 hours depending upon individual healing capacity and hormonal status.
The regenerative process involves rapid epithelial cell migration to cover microscopic defects, supported by enhanced local blood flow and inflammatory cell recruitment. This healing cascade explains why bleeding patterns often intensify briefly before gradually subsiding. Understanding these normal physiological responses helps distinguish expected outcomes from pathological bleeding requiring medical intervention.
Physiological mechanisms behind Post-Pap smear bleeding episodes
The mechanisms underlying post-cervical screening bleeding involve complex interactions between mechanical trauma, vascular architecture, and individual physiological factors. Research conducted by leading gynaecological pathology centres demonstrates that bleeding severity correlates with multiple variables, including cervical vascularity, hormonal status, and pre-existing inflammatory conditions. Understanding these mechanisms provides crucial context for both healthcare providers and patients when evaluating post-procedural symptoms.
Cervical vasculature disruption during speculum examination
The cervical vasculature comprises a rich network of capillaries and arterioles positioned immediately beneath the epithelial surface, making them particularly vulnerable to disruption during examination procedures. Speculum insertion and manipulation can compress these vessels, creating temporary ischaemia followed by reactive hyperaemia upon instrument removal. This vascular response, known as reactive bleeding, typically manifests as bright red spotting beginning shortly after the examination.
The degree of vascular disruption depends significantly upon speculum size selection and insertion technique. Oversized speculums or excessive opening pressure can compress larger vessels, leading to more pronounced bleeding episodes. Modern plastic speculums with rounded edges demonstrate reduced bleeding rates compared to traditional metal instruments , suggesting that equipment design plays a crucial role in minimising vascular trauma.
Squamocolumnar junction trauma and microhaemorrhage
The squamocolumnar junction represents the most mechanically sensitive area of the cervix due to the abrupt transition between different epithelial types. This anatomical boundary exhibits increased vascularity and reduced structural integrity compared to surrounding tissues, making it prone to microhaemorrhage during sampling procedures. The junction’s position varies significantly between individuals and can shift in response to hormonal fluctuations, pregnancy, and age-related changes.
Sampling instruments must traverse this transitional zone to ensure adequate cellular representation, inevitably creating microscopic disruptions to the epithelial architecture. These microtraumas heal rapidly under normal circumstances but can produce visible bleeding lasting 24-48 hours. The bleeding typically appears as light brown or pink discharge rather than bright red blood, reflecting the time required for haemoglobin breakdown in the cervical environment.
Hormonal influences on cervical tissue fragility
Oestrogen levels significantly influence cervical tissue characteristics, with higher concentrations promoting increased vascularity and epithelial thickness. Women in the proliferative phase of their menstrual cycle demonstrate enhanced bleeding propensity compared to those in the secretory phase, reflecting oestrogen-mediated vascular changes. Hormonal contraceptive users may exhibit altered bleeding patterns due to synthetic hormone effects on cervical architecture.
Pregnancy represents an extreme example of hormonal influence on cervical bleeding susceptibility. The dramatic increase in blood volume and vascular proliferation during gestation creates a highly friable cervical surface prone to bleeding with minimal manipulation. Pregnant women experience post-Pap bleeding rates approximately 40% higher than non-pregnant counterparts , though this bleeding remains clinically benign in the vast majority of cases.
Endocervical canal sensitivity and bleeding propensity
The endocervical canal’s columnar epithelium demonstrates greater mechanical sensitivity compared to the robust squamous epithelium covering the ectocervix. This increased fragility stems from the single-cell-layer thickness of columnar epithelium versus the multi-layered squamous arrangement. Consequently, endocervical sampling procedures carry higher bleeding risks, particularly in postmenopausal women where oestrogen deficiency further compromises epithelial integrity.
Individual variations in endocervical anatomy, including canal diameter and epithelial thickness, significantly influence bleeding susceptibility. Women with narrow cervical canals may experience more trauma during brush insertion, whilst those with ectropion (columnar epithelium extension onto the ectocervix) demonstrate increased bleeding propensity due to exposed fragile tissue.
Distinguishing normal spotting from concerning haemorrhage patterns
Differentiating between physiological post-procedural bleeding and pathological haemorrhage requires careful evaluation of multiple clinical parameters. Normal spotting typically exhibits specific characteristics that distinguish it from bleeding requiring medical intervention. Healthcare providers emphasise that normal post-Pap bleeding should be minimal, self-limiting, and resolve within 72 hours without intervention . Understanding these distinguishing features empowers women to make informed decisions about seeking additional medical care.
The volume, duration, colour, and associated symptoms of post-procedural bleeding provide crucial diagnostic information. Normal spotting rarely exceeds the equivalent of light menstrual flow and typically appears as pink or brown discharge rather than bright red blood. The bleeding pattern should demonstrate progressive reduction over time rather than increasing intensity or persistence beyond three days. Any deviation from these expected patterns warrants professional medical evaluation.
Clinical studies indicate that fewer than 2% of women experiencing post-Pap bleeding require active medical intervention, with the majority of cases representing normal physiological responses to cervical sampling procedures.
Concerning bleeding patterns include heavy flow requiring frequent pad changes, bright red blood with clots, bleeding persisting beyond 72 hours, or haemorrhage accompanied by severe cramping or pelvic pain. These symptoms may indicate underlying conditions such as cervical polyps, infections, or rarely, malignant processes requiring immediate evaluation. The timing of bleeding onset also provides diagnostic clues, with immediate bright red bleeding suggesting vascular trauma, whilst delayed bleeding may indicate infection or other pathological processes.
Women should monitor additional symptoms accompanying the bleeding, including fever, unusual vaginal discharge, or severe pelvic discomfort. The presence of these associated symptoms significantly increases the likelihood of underlying pathology requiring treatment. Foul-smelling discharge accompanying post-Pap bleeding may indicate bacterial infection necessitating antibiotic therapy . Temperature elevation above 38°C within 48 hours of cervical screening warrants immediate medical attention to exclude ascending infection.
Risk factors predisposing to increased Post-Screening bleeding
Multiple risk factors can predispose women to increased bleeding following cervical screening procedures, ranging from physiological conditions to medication effects. Pregnancy represents the most significant risk factor, with gestational changes creating a highly vascularised and friable cervical environment. Hormonal contraceptive use, particularly combined oral contraceptives, can increase bleeding susceptibility through effects on cervical vascularity and epithelial characteristics. Understanding these risk factors enables both healthcare providers and patients to anticipate potential bleeding episodes and implement appropriate management strategies.
Age-related factors significantly influence bleeding propensity, with postmenopausal women demonstrating increased susceptibility due to oestrogen deficiency-induced epithelial atrophy. Conversely, very young women may experience heightened bleeding due to immature cervical architecture and increased vascularity. Women with a history of cervical procedures, including previous biopsies or cryotherapy, may exhibit altered bleeding patterns due to scarring or architectural changes affecting normal healing responses.
Medical conditions affecting coagulation or vascular integrity can substantially increase post-procedural bleeding risk. Anticoagulant medications, including warfarin and direct oral anticoagulants, create obvious bleeding tendencies requiring careful monitoring following cervical examination. Women taking antiplatelet medications such as aspirin demonstrate bleeding rates approximately 30% higher than non-users , though the clinical significance remains minimal in most cases. Bleeding disorders, whilst rare, can manifest dramatically following seemingly minor cervical trauma.
Inflammatory conditions of the cervix, including cervicitis from infectious or non-infectious causes, significantly increase bleeding susceptibility by creating friable, hypervascular tissue prone to trauma. Human papillomavirus infection can alter cervical architecture, potentially increasing bleeding propensity during sampling procedures. Cervical ectropion, where columnar epithelium extends onto the ectocervix, creates visible bleeding tendencies due to the exposed fragile tissue surface.
Behavioural factors also influence bleeding patterns, with recent sexual activity potentially increasing cervical sensitivity and bleeding propensity. Douching or vaginal medication use immediately prior to examination can alter cervical epithelial integrity, affecting post-procedural bleeding patterns. Women who have undergone recent pelvic examinations or procedures demonstrate reduced bleeding rates, possibly due to tissue adaptation responses .
Clinical indicators requiring immediate gynaecological assessment
Recognising clinical indicators necessitating urgent gynaecological evaluation following cervical screening procedures is crucial for preventing serious complications and ensuring optimal patient outcomes. Heavy bleeding requiring hourly pad changes represents an absolute indication for immediate medical assessment, as it may indicate significant vascular injury or underlying pathology. The presence of large blood clots or tissue fragments in the discharge warrants prompt evaluation to exclude cervical trauma or concurrent pathological processes.
Severe pelvic pain accompanying post-procedural bleeding suggests possible complications beyond normal tissue trauma. This pain pattern may indicate cervical laceration, infection, or rarely, vasovagal responses requiring immediate intervention. Pain severity disproportionate to the minor nature of cervical sampling procedures consistently correlates with underlying pathological processes requiring treatment . Women experiencing difficulty with normal activities due to pain or bleeding should seek immediate medical attention.
Systemic symptoms including fever, chills, or generalised malaise accompanying post-Pap bleeding may indicate ascending infection requiring urgent antibiotic therapy. These symptoms typically develop 24-72 hours after the procedure and represent serious complications that can progress to pelvic inflammatory disease if left untreated. Blood pressure changes, dizziness, or fainting episodes associated with bleeding suggest significant blood loss or vasovagal responses requiring immediate medical evaluation.
The timing and progression of bleeding provide crucial diagnostic information regarding the need for urgent assessment. Bleeding that initially improves but then worsens after 24-48 hours may indicate delayed complications such as infection or delayed bleeding from deeper tissue trauma. Bleeding persisting beyond 72 hours without improvement consistently indicates pathological processes requiring intervention rather than normal physiological responses . Any bleeding accompanied by unusual or foul-smelling discharge warrants immediate evaluation for infectious complications.
Emergency department protocols recommend immediate gynaecological consultation for any woman experiencing heavy post-procedural bleeding accompanied by haemodynamic instability or signs of systemic infection.
Evidence-based aftercare protocols and bleeding management strategies
Contemporary aftercare protocols for post-cervical screening bleeding management emphasise patient education, symptom monitoring, and graduated intervention strategies based on bleeding severity and duration. Evidence-based guidelines recommend initial conservative management for light bleeding, including activity modification and hygiene precautions to prevent infection. Women should avoid tampon use for 48-72 hours following the procedure to prevent disruption of healing tissue and reduce infection risk. Sexual activity restriction for 24-48 hours allows adequate time for initial epithelial healing whilst minimising additional cervical trauma.
Pain management strategies focus on simple analgesics and heat application for cramping or discomfort. Paracetamol represents the first-line analgesic choice due to its lack of antiplatelet effects, whilst non-steroidal anti-inflammatory drugs should be used cautiously due to potential bleeding enhancement. Topical heat application to the lower abdomen provides effective symptom relief for cervical cramping without interfering with normal healing processes . Women experiencing significant discomfort should contact their healthcare provider for additional management options.
Hygiene protocols emphasise gentle cleansing with plain water and avoidance of perfumed products that might irritate healing tissues. Panty liners or light sanitary pads provide adequate protection for normal spotting whilst allowing monitoring of bleeding patterns. Women should track bleeding volume, colour, and associated symptoms to provide accurate information for healthcare providers if complications develop. Daily symptom logs help distinguish between normal healing progression and pathological bleeding requiring intervention.
Follow-up protocols recommend routine contact within 72 hours for women experiencing any post-procedural bleeding to assess symptom progression and provide reassurance. Healthcare providers should maintain low thresholds for additional evaluation given the potential for serious complications, whilst simultaneously providing appropriate reassurance for the majority of patients experiencing normal physiological responses. Structured telephone follow-up protocols have demonstrated effectiveness in reducing anxiety whilst ensuring appropriate identification of complications requiring treatment . These systematic approaches to post-procedural care optimise both patient safety and satisfaction whilst minimising unnecessary medical interventions for benign bleeding episodes.
Regular monitoring protocols incorporate patient education materials detailing warning signs that necessitate immediate medical contact. These educational resources should emphasize the importance of distinguishing between expected spotting and concerning bleeding patterns. Healthcare facilities implementing standardized aftercare protocols report significantly improved patient satisfaction scores and reduced rates of unnecessary emergency department visits for benign post-procedural symptoms.
Documentation requirements for post-screening bleeding episodes include detailed recording of bleeding characteristics, associated symptoms, and patient risk factors. This systematic documentation enables healthcare providers to identify patterns predicting bleeding complications and refine their sampling techniques accordingly. Electronic health record integration of bleeding assessment tools facilitates consistent monitoring whilst providing valuable data for quality improvement initiatives . Comprehensive documentation also supports medicolegal protection should complications develop requiring additional interventions.
Patient communication strategies focus on pre-procedural counseling regarding expected post-screening symptoms and appropriate management responses. Clear verbal and written instructions regarding activity restrictions, hygiene protocols, and warning signs requiring immediate medical attention significantly reduce patient anxiety and improve compliance with aftercare recommendations. Healthcare providers should emphasize that mild bleeding represents a normal physiological response rather than a complication, whilst simultaneously educating patients about genuine warning signs necessitating urgent evaluation.
Research-based protocols continue evolving based on emerging evidence regarding optimal post-procedural management strategies. Recent studies investigating novel hemostatic agents and improved sampling techniques show promise for reducing bleeding rates whilst maintaining diagnostic accuracy. These advancing protocols aim to minimize patient discomfort and complications whilst preserving the screening effectiveness that makes cervical cytology such a valuable cancer prevention tool.
Contemporary evidence-based aftercare protocols have demonstrated a 40% reduction in patient anxiety levels and a 25% decrease in unnecessary follow-up appointments for benign post-procedural bleeding episodes.