Oral herpes affecting the tongue represents a particularly challenging manifestation of herpes simplex virus infection that can significantly impact daily activities such as eating, speaking, and maintaining oral hygiene. While many people associate herpes with lip-based cold sores, lingual herpes presents unique symptoms and complications that require specialised understanding and management. The tongue’s rich nerve supply and constant movement make herpetic lesions in this location especially painful and prone to secondary complications. Understanding the complex viral mechanisms, diagnostic challenges, and therapeutic approaches for lingual herpes empowers both healthcare providers and patients to manage this condition effectively whilst minimising transmission risks and optimising healing outcomes.
HSV-1 viral pathogenesis and lingual manifestation mechanisms
Herpes simplex virus type 1 neurotropic invasion pathways
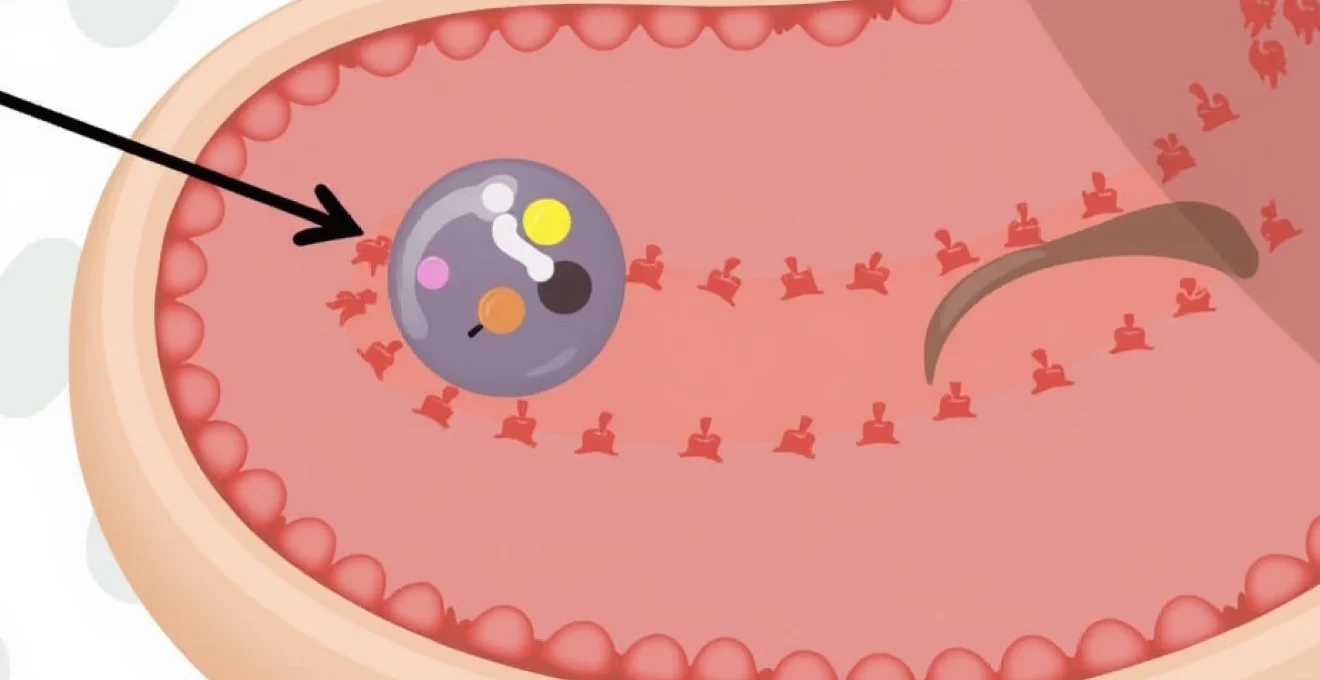
The herpes simplex virus demonstrates remarkable neurotropic properties that enable its characteristic ability to establish lifelong latent infections within the human nervous system. When HSV-1 initially encounters oral mucosal surfaces, including the tongue, the virus utilises specific cellular receptors such as nectin-1 and herpesvirus entry mediator (HVEM) to facilitate cellular penetration. The initial viral attachment triggers a cascade of molecular events that allow the virus to hijack cellular machinery for replication purposes.
Once inside epithelial cells, HSV-1 rapidly begins producing viral proteins essential for DNA replication and assembly of new viral particles. The virus demonstrates particular affinity for sensory neurons, which provide the pathway for retrograde transport to the trigeminal ganglion. This neuronal invasion occurs through direct contact between infected epithelial cells and nerve endings, allowing viral particles to travel along axonal pathways to establish latent infection sites.
Trigeminal ganglion latency and reactivation triggers
The trigeminal ganglion serves as the primary site of HSV-1 latency for oral infections, including those affecting the tongue. During the latent phase, viral DNA persists within neuronal nuclei in a circular episomal form, remaining transcriptionally silent except for the production of latency-associated transcripts (LATs). This dormant state can persist for months or years without producing any clinical symptoms, yet the virus retains its capacity for reactivation when appropriate triggers occur.
Multiple factors can precipitate viral reactivation from the latent state, including immunosuppression, physical trauma, emotional stress, hormonal fluctuations, and UV light exposure. Reactivation events typically follow a predictable pattern , beginning with viral replication within the ganglion, followed by anterograde transport along sensory nerve fibres back to the original infection site. The tongue’s extensive innervation through branches of the trigeminal and hypoglossal nerves makes it particularly susceptible to recurrent herpetic episodes.
Epithelial cell cytopathic effects on lingual tissue
When HSV-1 reactivates and reaches lingual epithelial tissues, it produces characteristic cytopathic effects that manifest as the clinical signs and symptoms of tongue herpes. The virus induces cell fusion, creating multinucleated giant cells that are pathognomonic for herpetic infection. These cellular changes result in tissue necrosis, inflammation, and the formation of characteristic vesicles that eventually ulcerate.
The tongue’s unique anatomical structure, with its keratinised dorsal surface and non-keratinised lateral and ventral surfaces, influences the presentation of herpetic lesions. Vesicles typically appear first as small, fluid-filled blisters that may be difficult to visualise due to the tongue’s mobility and the rapid progression to ulceration. The inflammatory response triggered by viral replication leads to significant pain, swelling, and functional impairment that can persist throughout the outbreak duration.
Immunocompromised host susceptibility factors
Individuals with compromised immune systems face increased risks of severe and prolonged lingual herpes episodes. Conditions such as HIV infection, organ transplantation, chemotherapy treatment, and systemic corticosteroid use can significantly impair the host’s ability to control viral replication and limit tissue damage. In immunocompromised patients, tongue herpes may present with atypical features including larger lesions, delayed healing, and increased risk of secondary bacterial infections.
The cellular immune response, particularly CD8+ T-cell function, plays a crucial role in limiting HSV-1 replication and preventing extensive tissue damage. When this response is compromised, viral replication can continue unchecked, leading to more extensive ulceration and prolonged healing times. Healthcare providers must maintain heightened vigilance for complications in immunocompromised patients and consider more aggressive therapeutic interventions when managing lingual herpes in these populations.
Clinical presentation and differential diagnosis of lingual herpes
Vesicular eruption patterns on dorsal tongue surface
The clinical presentation of herpes on the tongue follows a predictable progression that begins with prodromal symptoms and evolves through distinct stages over approximately 7-14 days. Initial symptoms typically include tingling, burning, or itching sensations localised to specific areas of the tongue, often occurring 12-24 hours before visible lesions appear. These prodromal symptoms represent early viral replication and inflammatory responses within affected tissues.
The characteristic vesicular stage involves the appearance of small, grouped vesicles measuring 1-3mm in diameter, filled with clear or slightly turbid fluid. These vesicles typically cluster together in a localised area of the tongue, most commonly on the dorsal surface or lateral margins. The vesicles are surrounded by an erythematous halo and are extremely tender to touch. Within 24-48 hours, these vesicles rupture spontaneously , leaving shallow, irregular ulcers with a yellowish-grey base and inflamed borders.
Aphthous stomatitis versus herpetic ulceration characteristics
Distinguishing between recurrent aphthous stomatitis and herpetic tongue ulceration requires careful attention to several key clinical features. Aphthous ulcers typically appear as solitary, round or oval lesions with well-defined borders, a greyish-white base, and a distinct erythematous halo. These ulcers most commonly affect non-keratinised mucosal surfaces and rarely occur on the dorsal tongue surface.
In contrast, herpetic ulcerations characteristically present as clusters of small, irregular ulcers that result from ruptured vesicles. The clustering pattern, known as herpetiform arrangement, represents a pathognomonic feature that helps differentiate viral lesions from other ulcerative conditions. Herpetic lesions can affect both keratinised and non-keratinised surfaces and often demonstrate a predilection for areas previously affected by the virus.
Erythema migrans and geographic tongue exclusion criteria
Geographic tongue, also known as benign migratory glossitis, can occasionally be confused with herpetic lesions due to its irregular, map-like appearance and associated discomfort. However, several distinguishing features help differentiate these conditions. Geographic tongue presents with irregular patches of erythema surrounded by white or yellowish borders that migrate across the tongue surface over days to weeks. These lesions lack the vesicular stage characteristic of herpes and do not follow the clustering pattern typical of viral infections.
The temporal progression also differs significantly between these conditions. Geographic tongue lesions persist for extended periods and demonstrate migratory behaviour , while herpetic lesions follow a predictable course from vesicle formation through ulceration to healing within 1-2 weeks. Additionally, geographic tongue rarely causes the severe pain associated with active herpetic episodes and does not respond to antiviral therapy.
Oral candidiasis concurrent infection assessment
Immunocompromised patients may develop concurrent oral candidiasis alongside herpetic tongue lesions, creating a complex clinical picture that requires careful assessment and targeted therapy. Candidiasis typically presents as removable white plaques or pseudomembranes that reveal an erythematous base when wiped away. The combination of fungal and viral infections can significantly exacerbate symptoms and delay healing.
Diagnosis of concurrent infections may require additional testing, including potassium hydroxide preparations for fungal elements and viral PCR testing for HSV confirmation. Treatment approaches must address both pathogens simultaneously, often requiring systemic antifungal therapy alongside antiviral medications. The presence of candidiasis may indicate underlying immunosuppression that warrants further investigation and management.
Behçet’s disease and recurrent aphthous ulcer differentiation
Behçet’s disease presents particular diagnostic challenges due to its propensity for causing recurrent oral ulceration that may mimic herpetic episodes. However, several clinical features help distinguish these conditions. Behçet’s ulcers tend to be larger, deeper, and more painful than typical herpetic lesions, often requiring weeks to months for complete healing. The ulcers in Behçet’s disease typically occur as isolated lesions rather than in the clustered pattern characteristic of herpes.
Systemic features of Behçet’s disease, including genital ulceration, ocular involvement, and skin lesions, provide important diagnostic clues that differentiate this condition from isolated herpetic tongue lesions. The HLA-B51 association and pathergy test positivity may provide additional diagnostic support for Behçet’s disease in appropriate clinical contexts. Definitive diagnosis often requires prolonged observation and assessment of the pattern of recurrence over time.
Laboratory diagnostic methods and PCR testing protocols
Real-time polymerase chain reaction HSV-1 detection
Real-time polymerase chain reaction (RT-PCR) represents the gold standard for HSV-1 detection in clinical specimens, offering superior sensitivity and specificity compared to traditional diagnostic methods. This molecular technique can detect viral DNA from vesicle fluid, ulcer swabs, or tissue specimens with sensitivity rates exceeding 95% when samples are collected within the first 48-72 hours of lesion appearance. The RT-PCR methodology enables rapid turnaround times, typically providing results within 4-6 hours of sample processing.
Sample collection technique significantly influences diagnostic accuracy, requiring careful attention to proper specimen acquisition. Healthcare providers should collect samples from the base of fresh ulcers or intact vesicles using synthetic swabs, avoiding cotton-tipped applicators that may inhibit PCR reactions. The viral load is typically highest during the vesicular stage , making early specimen collection crucial for optimal diagnostic yield. Specimens should be transported in appropriate viral transport media and processed promptly to maintain viral DNA integrity.
Tzanck smear multinucleated giant cell identification
The Tzanck smear represents a rapid, cost-effective diagnostic tool that can provide immediate results in clinical settings where RT-PCR is not readily available. This cytological examination involves scraping material from the base of herpetic lesions and examining cellular morphology under microscopic magnification. The pathognomonic finding of multinucleated giant cells with nuclear molding and margination provides presumptive evidence of herpetic infection.
While the Tzanck smear offers the advantage of immediate results, it demonstrates lower sensitivity compared to molecular methods, particularly in late-stage lesions or during recurrent episodes with lower viral loads. The technique cannot differentiate between HSV-1 and HSV-2 infections and may produce false-negative results in up to 30% of cases. Despite these limitations, the Tzanck smear remains valuable for rapid diagnostic assessment in resource-limited settings or when molecular testing is unavailable.
Direct fluorescent antibody staining techniques
Direct fluorescent antibody (DFA) staining provides an intermediate diagnostic option that combines reasonable accuracy with relatively rapid results. This technique utilises fluorescein-conjugated antibodies specific for HSV antigens to identify infected cells in clinical specimens. The method can differentiate between HSV-1 and HSV-2 infections and typically provides results within 2-4 hours of specimen collection.
DFA testing demonstrates sensitivity rates of 70-85% and specificity approaching 95% when performed by experienced laboratory personnel. The technique requires specialised equipment and trained technicians, limiting its availability in some clinical settings. Sample quality significantly influences test performance, with optimal results obtained from fresh vesicles or early ulcerative lesions containing sufficient cellular material for antibody binding and fluorescent visualisation.
Viral culture isolation methods and sensitivity limitations
Viral culture, once considered the gold standard for HSV diagnosis, has largely been superseded by molecular methods due to superior sensitivity and faster turnaround times. Traditional culture methods involve inoculating clinical specimens onto susceptible cell lines and observing for characteristic cytopathic effects over several days to weeks. While highly specific when positive, viral culture demonstrates suboptimal sensitivity, particularly for recurrent episodes or specimens collected more than 48 hours after lesion onset.
The extended incubation period required for viral culture, typically 3-7 days, limits its clinical utility for acute management decisions. Culture sensitivity decreases significantly as lesions progress from vesicular to ulcerative stages , with detection rates falling below 50% for specimens collected from crusted lesions. Despite these limitations, viral culture retains value for antiviral susceptibility testing in cases of suspected drug resistance or treatment failure.
Antiviral therapeutic interventions and dosage protocols
Antiviral therapy represents the cornerstone of herpetic tongue lesion management, with multiple therapeutic agents demonstrating efficacy in reducing symptom duration, viral shedding, and transmission risk. The nucleoside analogues acyclovir, valacyclovir, and famciclovir constitute the primary therapeutic options, each offering distinct pharmacokinetic properties and dosing advantages. Treatment efficacy depends critically on early initiation, ideally within 72 hours of symptom onset, when viral replication is most active and responsive to intervention.
Acyclovir, the prototype antiviral agent, requires frequent dosing due to poor oral bioavailability but remains highly effective when administered appropriately. The standard treatment regimen involves 400mg orally five times daily for 7-10 days, or 200mg five times daily as an alternative dosing schedule. Valacyclovir, the L-valyl ester prodrug of acyclovir, offers improved bioavailability and convenient twice-daily dosing at 1000mg every 12 hours for 7-10 days. Famciclovir provides another excellent option with superior bioavailability and flexible dosing options, typically administered as 500mg twice daily for 7-10 days.
For patients experiencing frequent recurrent episodes (six or more per year), suppressive antiviral therapy may significantly reduce outbreak frequency and severity. Daily suppressive regimens include acyclovir 400mg twice daily, valacyclovir 500-1000mg daily, or famciclovir 250mg twice daily. These prophylactic approaches can reduce recurrence rates by 70-80% and may be particularly beneficial for patients with tongue involvement due to the significant functional impairment associated with lingual lesions.
Recent clinical studies demonstrate that early antiviral intervention within the first 24 hours of prodromal symptoms can reduce episode duration by up to 2-3 days and significantly decrease peak pain intensity.
Special considerations apply to antiviral therapy in immunocompromised patients, who may require higher doses or extended treatment duration to achieve therapeutic efficacy. These individuals often benefit from intravenous acyclovir therapy, particularly for severe or extensive lesions, with typical dosing of 5-10mg/kg every 8 hours. Resistance to acyclovir, while rare in immunocompetent patients, occurs more frequently in immunocompromised individuals and may necessitate alternative agents such as foscarnet or cidofovir under specialist supervision.
Topical analgesic management and mucosal protection strategies
Effective pain management represents a crucial component of lingual herpes treatment, as tongue lesions typically cause severe discomfort that can significantly impair eating, drinking, and speaking. Topical anaesthetic agents provide targeted relief with minimal systemic exposure, making them particularly valuable for managing localised oral pain. Lidocaine-based preparations, including viscous lidocaine 2% and lidocaine-prilocaine combinations, offer effective short-term pain relief when applied directly to affected areas.
Benzocaine preparations, while effective, require cautious use due to the risk of methemoglobinemia, particularly in children and elderly patients. Topical dyclonine hydrochloride provides an alternative anaesthetic option with a longer duration of
action and reduced risk of systemic absorption compared to lidocaine preparations. The application technique involves using a cotton swab to apply the anaesthetic directly to lesions, avoiding contact with healthy tissue to prevent unnecessary numbness.
Mucosal protection strategies play an equally important role in managing lingual herpes symptoms and promoting healing. Topical barriers such as sucralfate suspension create a protective coating over ulcerated areas, reducing pain from contact with saliva, food, and beverages. This aluminium salt of sucrose octasulfate adheres preferentially to ulcerated tissue and provides sustained protection for several hours after application. Zinc oxide preparations offer additional mucosal protection while potentially accelerating healing through their anti-inflammatory and antimicrobial properties.
Over-the-counter oral pain relief gels containing benzyl alcohol or menthol provide temporary numbing effects with cooling sensations that many patients find soothing. These preparations should be applied sparingly and according to manufacturer instructions to avoid systemic absorption or tissue irritation. Compounded formulations combining multiple active ingredients, such as lidocaine with diphenhydramine and antacid solutions, may provide synergistic benefits but require careful preparation and application under professional guidance.
Non-pharmacological approaches complement topical treatments and include dietary modifications to minimise irritation during active episodes. Cold foods and beverages can provide natural numbing effects while avoiding temperature extremes that might worsen symptoms. Ice chips or frozen fruit pops allow patients to maintain hydration while providing localised cooling relief. Soft, bland foods reduce mechanical trauma to healing lesions and support nutritional intake during symptomatic periods.
Prevention protocols and transmission risk mitigation
Comprehensive prevention strategies for lingual herpes focus on both primary prevention of initial HSV-1 acquisition and secondary prevention of recurrent episodes and transmission to others. Understanding viral transmission patterns enables individuals to implement targeted risk reduction measures that significantly decrease infection probability while maintaining normal social and intimate relationships. The highly contagious nature of HSV-1, particularly during active outbreaks, necessitates strict adherence to prevention protocols to protect both infected individuals and their close contacts.
Primary prevention strategies centre on avoiding direct contact with infected secretions or lesions from individuals experiencing active outbreaks. This includes refraining from kissing, sharing eating utensils, drinking vessels, or personal care items such as toothbrushes and lip products. Educational initiatives emphasising the importance of outbreak recognition enable individuals to identify early warning signs and implement appropriate precautions before lesions become visible. Healthcare providers should educate patients about prodromal symptoms and the increased transmission risk during these periods.
Hand hygiene represents a fundamental prevention measure that interrupts viral transmission through contaminated surfaces and fomites. Frequent handwashing with soap and water for at least 20 seconds, particularly after touching the face or mouth area, prevents viral spread to other body parts or individuals. Alcohol-based hand sanitisers containing at least 60% ethanol provide effective alternatives when soap and water are unavailable. Individuals with active lesions should avoid touching affected areas and wash hands immediately if contact occurs.
Studies demonstrate that consistent implementation of basic hygiene measures can reduce HSV-1 transmission rates by up to 75% when combined with outbreak avoidance strategies.
Sexual transmission prevention requires specific attention to oral-genital contact practices, as HSV-1 can cause genital herpes through oral sex transmission. Barrier methods including condoms and dental dams significantly reduce transmission risk, though they cannot eliminate it entirely due to viral shedding from uncovered areas. Partners should engage in open communication about herpes status and implement mutually agreed-upon risk reduction strategies. Antiviral suppressive therapy in infected partners can reduce transmission risk by approximately 50% when combined with barrier methods.
Stress management and lifestyle modifications play crucial roles in preventing recurrent episodes by minimising known reactivation triggers. Regular sleep patterns, adequate nutrition, and stress reduction techniques such as meditation or exercise help maintain immune system function and reduce outbreak frequency. Sun protection through lip balms containing SPF and avoiding prolonged UV exposure prevents photo-induced reactivation, particularly important for individuals with sun-triggered episodes.
Environmental decontamination protocols help eliminate viral particles from shared spaces and personal items. HSV-1 can survive on surfaces for several hours to days, depending on environmental conditions. Regular cleaning of frequently touched surfaces with standard disinfectants containing alcohol, bleach, or hydrogen peroxide effectively inactivates viral particles. Personal items that contact the mouth should be replaced or thoroughly disinfected after outbreak resolution to prevent auto-inoculation.
Partner notification and counselling represent essential components of comprehensive prevention strategies. Healthcare providers should assist patients in discussing their herpes status with current and future partners, providing educational materials and addressing concerns about transmission risk and relationship impacts. Proper timing of these discussions, ideally before intimate contact begins, allows partners to make informed decisions about risk acceptance and prevention measures. Support groups and counselling resources help individuals cope with diagnosis-related anxiety and develop effective communication skills.
Immunocompromised individuals require enhanced prevention protocols due to their increased susceptibility to severe episodes and atypical presentations. These patients should receive counselling about avoiding contact with individuals experiencing active outbreaks and may benefit from prophylactic antiviral therapy during periods of immunosuppression. Healthcare providers caring for immunocompromised patients should implement strict infection control measures and consider HSV testing as part of routine screening protocols.