Morning occipital pain affects millions of people worldwide, transforming what should be a refreshing start to the day into an uncomfortable experience. This distinctive type of head pain, localised to the posterior region of the skull, differs significantly from typical headaches in both its presentation and underlying mechanisms. Understanding the complex interplay between sleep positioning, anatomical structures, and various medical conditions becomes crucial for addressing this common yet often misunderstood phenomenon.
The occipital region houses numerous sensitive structures, including nerve pathways, muscle attachments, and joint complexes that can contribute to morning discomfort. Research indicates that approximately 30% of adults experience some form of morning headache, with occipital pain representing a significant subset of these cases. The multifactorial nature of this condition requires a comprehensive understanding of the various contributing elements to develop effective management strategies.
Anatomical structures contributing to occipital morning pain
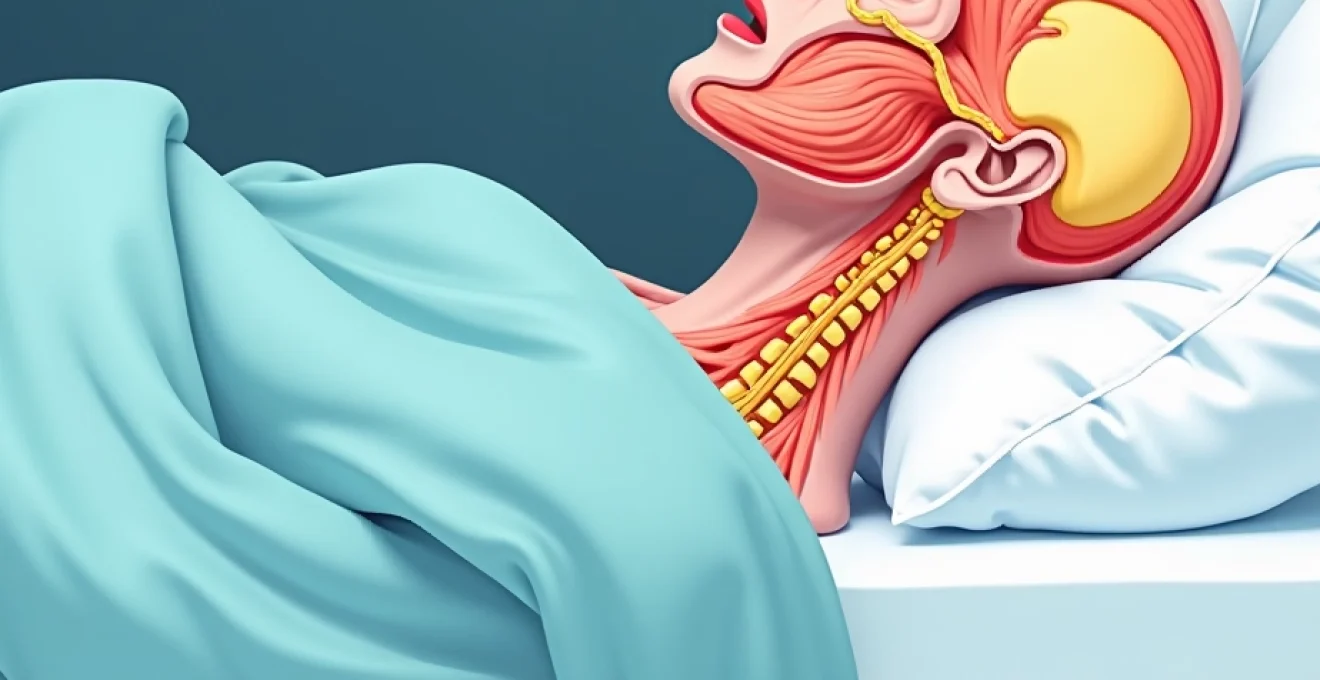
The posterior aspect of the skull contains several interconnected anatomical components that can generate pain when compromised. These structures work in harmony during normal function but can become sources of discomfort when subjected to prolonged stress or abnormal positioning during sleep. The complexity of this anatomical region explains why occipital pain often presents with varying characteristics and intensities.
Suboccipital muscle group tension and trigger points
The suboccipital muscle group comprises four small but powerful muscles that connect the upper cervical vertebrae to the occipital bone. These muscles include the rectus capitis posterior major and minor, along with the obliquus capitis superior and inferior. During sleep, particularly when cervical alignment is compromised, these muscles can develop trigger points and sustained tension that manifests as morning occipital pain.
Trigger points within the suboccipital muscles often refer pain in characteristic patterns, creating a band-like sensation across the posterior skull. The rectus capitis posterior major, when containing active trigger points, typically refers pain from the suboccipital region forward toward the temporal area. This referral pattern explains why many individuals experience pain that seems to wrap around their head upon waking.
Greater occipital nerve entrapment mechanisms
The greater occipital nerve emerges from the C2 nerve root and travels through multiple anatomical structures before innervating the posterior scalp. This nerve passes through the tendinous insertions of the trapezius and splenius capitis muscles, creating potential entrapment sites. When these muscles become hypertonic during sleep due to poor positioning or stress, they can compress the nerve, resulting in characteristic shooting or burning pain upon awakening.
Nerve entrapment symptoms typically present as sharp, electric-like sensations that may be triggered by light touch or hair brushing. The pain often follows the distribution of the nerve, extending from the suboccipital region toward the vertex of the skull. Understanding this anatomical relationship helps explain why some individuals experience scalp tenderness alongside their morning headaches.
Cervical spine C1-C2 atlantoaxial joint dysfunction
The atlantoaxial joint complex, consisting of the atlas (C1) and axis (C2) vertebrae, represents one of the most mobile segments of the spine. This joint allows for approximately 50% of cervical rotation and maintains crucial relationships with surrounding musculature and neural structures. When sleep positioning creates prolonged asymmetrical stress on this joint, morning occipital pain frequently results.
Dysfunction at the C1-C2 level can create referred pain patterns that extend into the occipital region through both mechanical and neurological pathways. The close proximity of the atlantoaxial joint to the greater occipital nerve explains why joint dysfunction often presents with both deep aching pain and superficial nerve-like symptoms. Sleep positions that maintain cervical rotation or side-bending can perpetuate this dysfunction.
Temporomandibular joint referred pain patterns
The temporomandibular joint (TMJ) demonstrates complex referred pain patterns that can extend into the occipital region. Nocturnal bruxism or clenching, often exacerbated by stress or sleep disorders, can create sustained tension in the muscles of mastication. The masseter, temporalis, and pterygoid muscles, when hypertonic, can refer pain through trigeminovascular pathways to the posterior head region.
The connection between jaw dysfunction and occipital pain highlights the interconnected nature of cranial structures. Sleep-related jaw clenching often intensifies during REM sleep phases, creating sustained muscle tension that persists into the morning hours. This mechanism explains why some individuals notice their occipital pain improves throughout the day as jaw muscles gradually relax.
Sleep Position-Related biomechanical factors
Sleep positioning plays a fundamental role in maintaining or disrupting the natural biomechanical relationships of the cervical spine and occipital region. Each sleep position creates unique stress patterns on anatomical structures, with some positions predisposing individuals to morning occipital pain more than others. Understanding these biomechanical principles enables targeted interventions for pain prevention.
Cervical lordosis alteration during supine sleep
The natural cervical lordosis, or forward curve of the neck, requires proper support during supine sleep to maintain optimal positioning. When pillows are too high or too low, the cervical curve becomes altered, creating compensatory tension in the suboccipital muscles. Excessive cervical flexion from overly thick pillows forces the suboccipital muscles into a shortened position, while inadequate support allows excessive extension.
Research demonstrates that maintaining neutral cervical alignment during supine sleep reduces morning neck pain by up to 60%. The ideal pillow height for supine sleepers should maintain the cervical curve while keeping the head in neutral alignment with the thoracic spine. Proper spinal alignment during sleep acts like a reset button for muscular tension accumulated during daily activities.
Lateral decubitus position and atlas rotation
Side sleeping, while often comfortable, creates unique challenges for cervical spine alignment. The lateral decubitus position requires careful attention to pillow height to prevent lateral flexion of the cervical spine. When the pillow is too thin, the head drops toward the supporting shoulder, creating lateral flexion and rotation at the atlantoaxial joint. Conversely, excessively thick pillows create lateral flexion toward the ceiling.
Atlas rotation in the lateral position commonly occurs when pillows fail to fill the shoulder-to-head distance adequately. This rotation can compress the greater occipital nerve on the dependent side while creating excessive stretch on the contralateral suboccipital muscles. The resulting muscle imbalances often manifest as unilateral morning occipital pain that corresponds to the preferred sleeping side.
Prone sleeping and cervical extension strain
Prone sleeping presents the most challenging position for cervical spine health, requiring sustained rotation and extension to maintain an airway. This position places the cervical spine in a mechanically disadvantaged position for extended periods, often resulting in morning stiffness and occipital pain. The sustained rotation required for prone sleeping creates asymmetrical stress on the atlantoaxial joint and associated musculature.
The extension component of prone sleeping particularly affects the suboccipital muscles, which must maintain sustained contraction to support the head against gravity. This sustained muscle activity throughout the night prevents the natural muscle relaxation that occurs during other sleep positions. Prone sleeping essentially creates an eight-hour isometric exercise for the neck muscles.
Pillow height impact on craniocervical alignment
Pillow height represents a critical variable in maintaining optimal craniocervical alignment across all sleep positions. The ideal pillow height varies significantly between individuals based on shoulder width, preferred sleep position, and existing cervical curvature. Mathematical models suggest that optimal pillow height should maintain the cervical spine in neutral alignment while supporting the natural lordotic curve.
Measurement techniques for determining proper pillow height involve assessing the distance from the lateral neck to the supporting surface in the lateral position, or from the posterior occiput to the supporting surface in supine positions. These measurements provide objective guidelines for pillow selection, though individual comfort preferences may require slight modifications to these calculated dimensions.
Pillow technology and ergonomic support systems
Advances in sleep technology have revolutionised pillow design, offering increasingly sophisticated solutions for maintaining optimal cervical alignment during sleep. Modern pillow systems incorporate various materials, contours, and adjustability features designed to address the complex biomechanical requirements of different sleep positions. Understanding these technological advances enables informed decisions about sleep surface modifications.
Memory foam contour pillow specifications for cervical support
Memory foam contour pillows utilise viscoelastic materials that respond to body heat and pressure to create customised support. The typical contour design features a lower section for the head and raised sections to support the cervical curve. High-quality memory foam pillows maintain consistent support throughout the night while conforming to individual anatomical variations.
Density specifications for therapeutic memory foam typically range from 4-5 pounds per cubic foot, providing adequate support while allowing sufficient contouring. The contouring properties of memory foam help distribute pressure evenly across the occipital region, reducing localised pressure points that can contribute to morning pain. Quality memory foam pillows often require a brief adjustment period as muscles adapt to proper alignment.
Latex vs polyurethane fill material properties
Natural latex and polyurethane foam materials offer different characteristics that affect their suitability for cervical support applications. Latex provides more responsive support, quickly returning to its original shape when pressure is removed, while polyurethane foams tend to have slower recovery times. These material properties influence how well pillows maintain support throughout the night as sleep positions change.
Latex pillows typically offer better temperature regulation due to their open cell structure, which allows for increased airflow. This temperature regulation can improve sleep quality and reduce the likelihood of position changes that disrupt cervical alignment. Polyurethane foams may retain more heat but often provide better pressure distribution for individuals with specific pressure point sensitivities.
Cervical roll integration and lordotic curve maintenance
Cervical rolls represent specialised pillow components designed specifically to support the natural lordotic curve of the cervical spine. These rolls can be integrated into standard pillows or used as standalone supports, particularly beneficial for supine sleepers who experience morning occipital pain. The diameter and firmness of cervical rolls must be carefully matched to individual anatomy to provide optimal support.
Proper cervical roll placement typically positions the roll at the level of the C3-C5 vertebrae, supporting the apex of the cervical lordosis. This positioning helps maintain the natural curve while preventing excessive flattening or reversal of the lordosis during sleep. Cervical rolls work like architectural supports, maintaining structural integrity while allowing natural movement.
Temperature-regulating materials and sleep quality correlation
Temperature regulation plays a crucial role in sleep quality and, consequently, in the development of morning occipital pain. Elevated head and neck temperatures can lead to increased restlessness and position changes, disrupting optimal cervical alignment throughout the night. Modern pillow materials incorporate various technologies to address temperature regulation challenges.
Phase-change materials, gel infusions, and copper-infused foams represent current technologies designed to maintain optimal sleeping temperatures. These materials help prevent the heat buildup that can occur with traditional memory foam, potentially improving sleep continuity and reducing the likelihood of position changes that compromise cervical alignment. Studies suggest that improved temperature regulation can reduce sleep disruptions by up to 40%.
Medical conditions manifesting as morning occipital pain
Several medical conditions can present with morning occipital pain as a primary symptom, requiring differentiation from simple mechanical causes. Sleep apnea represents one of the most common underlying conditions, with morning headaches affecting over 50% of individuals with this disorder. The intermittent hypoxia and carbon dioxide retention associated with apnea episodes can trigger vascular headaches that localise to the occipital region.
Cervicogenic headaches originate from dysfunction in the upper cervical spine and commonly present as morning occipital pain. These headaches result from referred pain mechanisms involving the trigeminocervical complex, which processes nociceptive input from both trigeminal and upper cervical sources. The characteristic unilateral nature and association with neck movement help distinguish cervicogenic headaches from other headache types.
Medication overuse headaches can manifest as morning occipital pain, particularly in individuals who regularly use analgesics before bedtime. The rebound effect from medication withdrawal during sleep hours can trigger headaches upon awakening.
Understanding medication patterns and their relationship to morning symptoms becomes crucial for proper diagnosis and treatment planning.
Hypertension occasionally presents with morning occipital headaches, particularly in cases of nocturnal blood pressure elevation. The pain typically correlates with blood pressure readings and may be accompanied by other symptoms such as visual disturbances or dizziness. Sleep-related breathing disorders often coexist with hypertension, creating a complex relationship between these conditions and morning head pain.
Diagnostic assessment techniques for morning head pain
Comprehensive assessment of morning occipital pain requires systematic evaluation of multiple potential contributing factors. Clinical history should focus on sleep patterns, pillow preferences, morning symptom characteristics, and associated symptoms such as sleep disruption or snoring. Detailed pain mapping helps identify specific anatomical structures involved and guides targeted interventions.
Physical examination should include assessment of cervical range of motion, suboccipital muscle tension, and neurological testing of the greater occipital nerve. Palpation of trigger points within the suboccipital muscles often reproduces familiar pain patterns. Joint mobility testing of the upper cervical spine can reveal restrictions that contribute to morning symptoms.
Sleep study evaluation may be warranted when morning headaches occur in conjunction with snoring, witnessed apneas, or excessive daytime sleepiness. Polysomnography can identify sleep-disordered breathing, sleep fragmentation, or other sleep disturbances that contribute to morning symptoms. Sleep studies provide objective data about physiological processes that occur during unconscious hours.
Imaging studies are typically reserved for cases with concerning features such as neurological deficits, progressive symptoms, or failure to respond to conservative measures. Magnetic resonance imaging can evaluate for structural abnormalities in the cervical spine or posterior fossa that might contribute to morning occipital pain. Plain radiographs may reveal atlantoaxial instability or other bony abnormalities affecting the upper cervical spine.
Evidence-based treatment protocols and prevention strategies
Treatment approaches for morning occipital pain should address both immediate symptom relief and long-term prevention strategies. Conservative management forms the foundation of treatment, focusing on sleep hygiene optimisation, ergonomic modifications, and targeted therapeutic interventions. The multifactorial nature of morning occipital pain often requires combination approaches for optimal outcomes.
Sleep position modification represents the most fundamental intervention for preventing morning occipital pain. Transitioning from prone to supine or lateral sleeping positions often provides significant symptom reduction within days to weeks. When lateral sleeping is preferred, proper pillow height adjustment becomes crucial for maintaining cervical alignment. Simple position changes can provide dramatic improvements in morning symptoms.
Therapeutic exercise programmes targeting the suboccipital muscles and upper cervical spine demonstrate significant efficacy in reducing morning occipital pain. Specific exercises include suboccipital releases, upper cervical strengthening, and postural correction techniques. Research indicates that consistent exercise programmes can reduce morning headache frequency by up to 70% within six weeks of implementation.
Manual therapy interventions, including suboccipital release techniques and upper cervical manipulation, provide both immediate and long-term benefits for individuals with morning occipital pain.
Trigger point therapy specifically targeting the suboccipital muscle group can provide rapid symptom relief and improve treatment outcomes when combined with other interventions. Dry needling or manual trigger point release techniques address the specific muscle dysfunctions that contribute to morning pain patterns. These treatments are most effective when combined with corrective exercises and sleep modifications.
Pharmacological interventions may be appropriate for individuals with severe symptoms or underlying medical conditions. Muscle relaxants taken before bedtime can help reduce nocturnal muscle tension, while anti-inflammatory medications address inflammatory components of cervicogenic headaches. However, medication timing requires careful consideration to avoid rebound effects that can worsen morning symptoms.
Stress management techniques play an important role in comprehensive treatment programmes, as psychological stress often exacerbates both sleep quality and muscle tension. Relaxation techniques, meditation, and cognitive behavioural therapy can improve both sleep quality and pain management outcomes. Regular stress reduction practices can reduce morning headache frequency by addressing one of the underlying perpetuating factors.