When you press gently on your teeth with your finger or tongue, you might notice they move slightly. This subtle movement is completely normal and occurs in even the healthiest mouths. Understanding why teeth exhibit this natural mobility requires examining the sophisticated biological systems that anchor teeth to the jawbone. Unlike rigid fixtures permanently cemented in place, teeth are held by a complex network of fibres, blood vessels, and nerve endings that allow for controlled movement while maintaining stability.
This physiological tooth movement serves important functions, from absorbing chewing forces to facilitating necessary adjustments during orthodontic treatment. The mechanisms behind tooth mobility involve intricate cellular processes, biomechanical responses, and adaptive changes that occur within the supporting structures. Natural tooth movement reflects the dynamic nature of oral tissues and their ability to respond to various stimuli whilst maintaining optimal function.
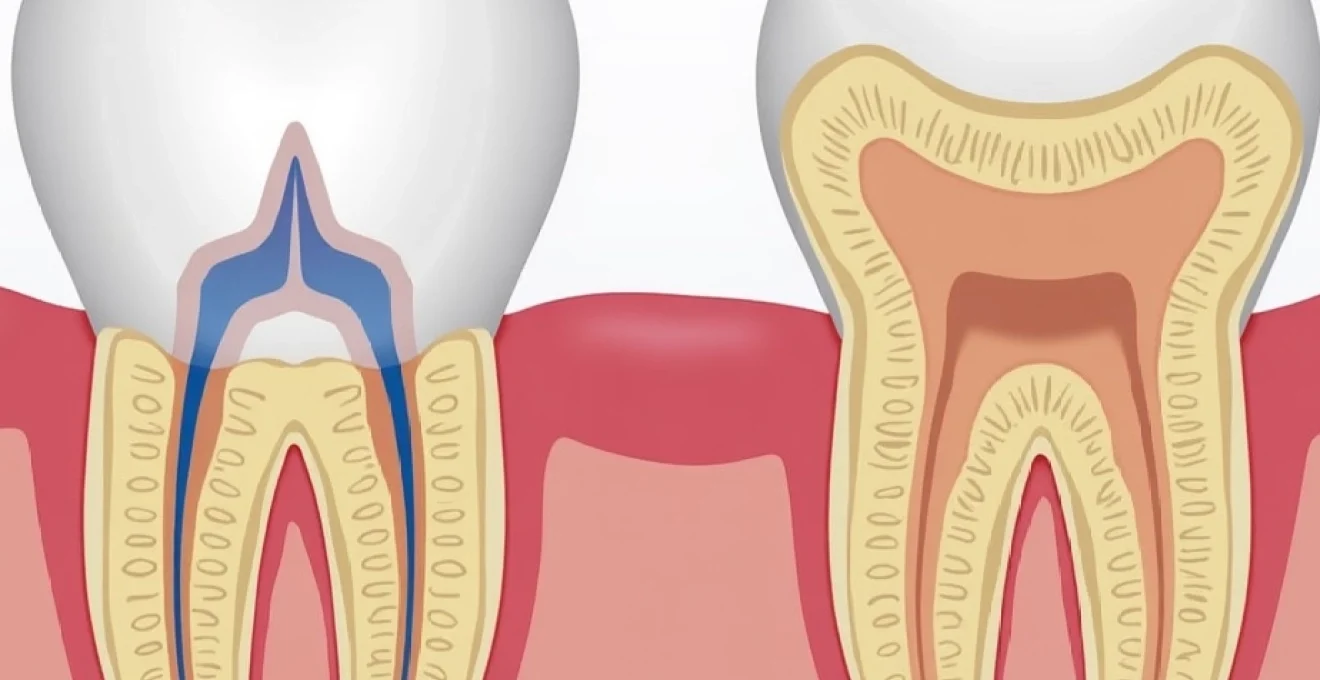
Periodontal ligament structure and tooth mobility mechanisms
The periodontal ligament serves as the primary cushioning system between each tooth root and the surrounding alveolar bone socket. This thin layer of connective tissue, measuring approximately 0.25 millimetres in width, contains a sophisticated arrangement of collagen fibres, blood vessels, and nerve endings that facilitate controlled tooth movement. The ligament’s unique structure allows teeth to move slightly under pressure whilst maintaining their position during normal function.
Collagen fibre arrangement in periodontal ligament space
The periodontal ligament contains several distinct groups of collagen fibres arranged in specific orientations to control different types of tooth movement. The principal fibres include alveolar crest fibres running horizontally, oblique fibres extending diagonally from the cementum to the alveolar bone, and apical fibres radiating from the root apex. This arrangement creates a suspension system that permits slight movement whilst resisting excessive displacement.
These fibres possess varying degrees of elasticity and tensile strength, allowing them to stretch under light pressure and return to their original position when the force is removed. Collagen turnover within the periodontal ligament occurs continuously, with new fibres being synthesised whilst older ones are broken down, maintaining the ligament’s adaptive capacity throughout life.
Sharpey’s fibres and cementum attachment points
Sharpey’s fibres represent specialised collagen bundles that embed directly into both the tooth’s cementum surface and the alveolar bone, creating strong anchoring points for the periodontal ligament. These mineralised fibres extend perpendicular to the root surface, providing secure attachment whilst allowing for controlled movement. The density and orientation of Sharpey’s fibres vary along different areas of the root surface, influencing movement patterns during orthodontic treatment.
The cementum layer covering the tooth root contains varying concentrations of these embedded fibres, with higher densities typically found in the cervical and apical regions. This distribution pattern contributes to the centre of resistance concept in orthodontics, where forces applied to the crown create predictable movement patterns based on the root’s attachment characteristics.
Vascular network response to applied pressure forces
The periodontal ligament contains an extensive network of blood vessels that respond dynamically to applied forces. When pressure is applied to a tooth, the vascular network experiences localised compression on one side of the root and tension on the opposite side. This vascular response triggers immediate changes in blood flow and tissue perfusion, influencing the cellular activities within the periodontal space.
The vascular changes also facilitate the transport of inflammatory mediators and cellular signalling molecules that coordinate the tissue remodelling process. Capillary compression on the pressure side can lead to localised hypoxia, whilst the tension side experiences increased blood flow and cellular activity, setting the stage for bone remodelling processes.
Proprioceptive nerve endings and mechanoreceptor function
Mechanoreceptors within the periodontal ligament detect even minimal changes in pressure and position, providing proprioceptive feedback about tooth position and movement. These specialised nerve endings respond to mechanical deformation of the ligament fibres, transmitting information to the central nervous system about bite force, tooth contact patterns, and potential threats to tooth integrity.
The mechanoreceptor response to applied pressure contributes to protective reflexes that prevent excessive force application and potential damage to tooth structures. This neurological feedback system helps explain why you can sense subtle tooth movement when applying gentle pressure with your finger or during orthodontic treatment.
Orthodontic force application and cellular response pathways
When orthodontic forces are applied to teeth, a complex cascade of cellular responses occurs within the periodontal ligament and surrounding bone. The initial application of force creates areas of compression and tension within the periodontal space, triggering specific cellular pathways that ultimately lead to tooth movement. Understanding these mechanisms helps explain why teeth move gradually during orthodontic treatment and why they can shift position even under light pressure.
Piezoelectric effect in alveolar bone during tooth movement
The piezoelectric effect occurs when mechanical stress applied to bone generates electrical potentials that influence cellular activity. In the context of tooth movement, compression of alveolar bone creates negative electrical charges, whilst tension areas develop positive charges. These electrical gradients serve as signals that guide osteoblast and osteoclast activity, directing bone formation and resorption processes respectively.
This bioelectrical phenomenon helps explain the precision of orthodontic tooth movement and why teeth tend to move in predictable directions when forces are applied. The piezoelectric response provides a mechanism for bones to adapt their structure in response to changing mechanical demands, facilitating controlled tooth repositioning whilst maintaining overall structural integrity.
Osteoblast and osteoclast activation through RANK-RANKL signalling
The RANK-RANKL signalling pathway represents a crucial mechanism for regulating bone remodelling during tooth movement. When orthodontic forces compress the periodontal ligament, local cells release RANKL (Receptor Activator of Nuclear factor Kappa-B Ligand), which binds to RANK receptors on osteoclast precursor cells. This binding promotes osteoclast differentiation and activation, leading to bone resorption on the compression side of the moving tooth.
Simultaneously, tension areas of the periodontal ligament experience decreased RANKL expression and increased osteoprotegerin production, which inhibits osteoclast formation and promotes osteoblast activity. This coordinated cellular response ensures that bone is removed where needed whilst new bone forms to fill spaces created by tooth movement, maintaining overall bone volume and structure.
Hyalinisation zones and undermining resorption processes
When orthodontic forces exceed the optimal range, hyalinisation zones can develop within the periodontal ligament. These areas appear as homogeneous, cell-free regions where the normal tissue architecture becomes disrupted due to excessive compression. Hyalinisation temporarily halts direct bone resorption and initiates a process called undermining resorption, where bone removal occurs from adjacent areas rather than directly beneath the compressed tissue.
This phenomenon explains why excessive orthodontic forces can actually slow tooth movement rather than accelerate it. Optimal force levels maintain cellular viability within the periodontal ligament whilst still triggering the necessary remodelling responses, ensuring efficient and comfortable tooth movement without tissue damage.
Prostaglandin E2 release and inflammatory cascade initiation
Prostaglandin E2 (PGE2) serves as a key inflammatory mediator released in response to orthodontic forces. This lipid compound increases vascular permeability, promotes vasodilation, and enhances the recruitment of inflammatory cells to the compressed periodontal ligament. PGE2 also directly stimulates osteoclast formation and activity whilst inhibiting osteoblast function, contributing to bone resorption on the pressure side of moving teeth.
The inflammatory cascade initiated by PGE2 release helps explain why teeth may feel tender or sensitive during the initial stages of orthodontic treatment. This inflammatory response is essential for tooth movement but can be modulated through various means, including the use of specific medications or force application techniques that minimise excessive tissue response.
Biomechanical properties of dental supporting structures
The biomechanical properties of teeth and their supporting structures determine how they respond to applied forces and why they exhibit natural mobility. The periodontal ligament functions as a complex shock-absorbing system with viscoelastic properties, meaning it demonstrates both elastic deformation and time-dependent flow characteristics when loaded. This combination allows teeth to move slightly under pressure whilst returning to their original position when the force is removed.
The elastic modulus of the periodontal ligament varies significantly depending on the loading rate and direction of applied force. Under rapid loading, such as during chewing, the ligament behaves more rigidly to protect the tooth from damage. However, under sustained light forces, the ligament exhibits more fluid-like properties that permit gradual tooth movement. This viscoelastic behaviour explains why orthodontic treatment requires continuous, gentle forces rather than intermittent heavy pressures.
The supporting alveolar bone also contributes significantly to tooth mobility characteristics. Cortical bone provides structural rigidity, whilst the trabecular bone offers more flexibility and adaptability. The ratio of cortical to trabecular bone varies throughout the jaw, influencing regional differences in tooth movement patterns. Areas with thinner cortical plates and more trabecular bone typically demonstrate greater natural tooth mobility.
Individual variations in periodontal ligament thickness, bone density, and tissue elasticity contribute to differences in tooth mobility between patients. Age-related changes also affect these biomechanical properties, with younger individuals typically showing greater tissue adaptability and faster orthodontic tooth movement compared to older adults. Understanding these variations helps explain why some people notice more tooth movement when applying pressure than others.
The remarkable adaptability of periodontal tissues allows teeth to respond to forces ranging from gentle finger pressure to the substantial loads generated during chewing, whilst maintaining their position and function throughout life.
Clinical applications in orthodontic treatment planning
Understanding natural tooth mobility mechanisms forms the foundation of modern orthodontic treatment planning. Orthodontists utilise knowledge of periodontal ligament properties and bone remodelling processes to design treatment strategies that achieve desired tooth movements efficiently and comfortably. The principles governing natural tooth mobility directly inform decisions about force magnitudes, treatment durations, and appliance designs used in contemporary orthodontic practice.
Light continuous forces versus heavy intermittent force systems
Contemporary orthodontic research consistently demonstrates that light continuous forces produce more efficient tooth movement than heavy intermittent forces. Light forces, typically ranging from 25-150 grams depending on the type of movement required, maintain cellular viability within the periodontal ligament whilst triggering appropriate remodelling responses. These forces work with the natural mobility characteristics of teeth rather than overwhelming the supporting tissues.
Heavy intermittent forces can cause extensive hyalinisation and undermining resorption, leading to prolonged treatment times and increased patient discomfort. The optimal force concept emphasises matching applied forces to the biological capacity of the periodontal tissues, ensuring continuous progress whilst minimising adverse effects such as root resorption or tissue damage.
Invisalign ClinCheck staging and incremental tooth movement
Modern clear aligner systems like Invisalign utilise sophisticated treatment planning software that breaks complex tooth movements into small incremental steps. Each aligner typically moves teeth approximately 0.25-0.33 millimetres per stage, working within the natural mobility limits of the periodontal ligament. This approach respects the biological principles of tooth movement whilst achieving predictable results.
The staging process considers the biomechanical properties of different tooth types and movement patterns, with more complex movements requiring smaller increments and longer treatment stages. Digital treatment planning allows for precise force calculations and movement predictions based on the individual patient’s anatomy and tissue responses.
Damon Self-Ligating brackets and reduced friction coefficients
Self-ligating bracket systems reduce friction between orthodontic wires and brackets, allowing teeth to move more freely in response to light forces. This reduced friction coefficient enables the natural mobility characteristics of teeth to be utilised more effectively, potentially reducing treatment times and improving patient comfort. The passive ligation system allows for more physiological tooth movement patterns.
The biomechanical advantages of reduced friction systems become particularly apparent during the alignment phase of treatment, where teeth can move more readily into proper position without the resistance created by conventional elastic or wire ligatures. This approach works in harmony with the natural periodontal ligament properties rather than fighting against them.
Pathological tooth mobility and periodontal disease progression
While normal physiological tooth mobility is expected and healthy, pathological mobility indicates underlying disease processes that compromise the supporting structures. Periodontal disease represents the most common cause of abnormal tooth mobility, progressively destroying the periodontal ligament, cementum, and alveolar bone that normally stabilise teeth. Understanding the distinction between normal and pathological mobility is crucial for maintaining oral health.
Miller classification system for gingival recession assessment
The Miller Classification system provides a standardised method for assessing gingival recession and its relationship to tooth mobility. Class I and II recession defects typically do not significantly affect tooth stability, as the underlying periodontal ligament and bone support remain intact. However, Class III and IV defects often involve loss of attachment and bone support, potentially leading to increased tooth mobility.
Progressive gingival recession can expose root surfaces and compromise the periodontal attachment apparatus, leading to gradual increases in tooth mobility over time. Attachment loss reduces the functional length of the periodontal ligament, decreasing its ability to stabilise the tooth and increasing susceptibility to movement under normal functional forces.
Furcation involvement and Multi-Rooted tooth stability
Multi-rooted teeth, including molars and some premolars, derive stability from their multiple root systems and the periodontal ligament attachments around each root. Furcation involvement occurs when periodontal disease affects the area between roots, compromising this multi-root support system. The progression from Class I through Class III furcation involvement correlates with increasing tooth mobility and decreased long-term prognosis.
The loss of inter-radicular bone and periodontal ligament significantly reduces the total attachment area available to stabilise these teeth. Even when individual roots maintain adequate support, furcation involvement can create areas of weakness that allow abnormal tooth movement patterns and reduced resistance to lateral forces during function.
Occlusal trauma and secondary periodontal ligament widening
Excessive occlusal forces can cause secondary widening of the periodontal ligament space, visible on radiographic examination as a thickened radiolucent line around the root surface. This widening represents the periodontal ligament’s attempt to accommodate increased functional demands but can also indicate the onset of pathological changes. Primary occlusal trauma occurs when excessive forces are applied to teeth with normal periodontal support, whilst secondary occlusal trauma involves normal forces applied to teeth with compromised support.
The relationship between occlusal trauma and tooth mobility is complex, with some degree of adaptation possible through increased periodontal ligament width and bone remodelling. However, when adaptive capacity is exceeded, progressive mobility and discomfort may develop. Clinical assessment must differentiate between adaptive responses and pathological changes requiring intervention to preserve tooth stability and function.
Recognising the difference between physiological tooth mobility and pathological movement patterns is essential for early intervention and preservation of long-term oral health.
The natural mobility of teeth when pushed reflects the remarkable biological engineering of the periodontal supporting apparatus. This sophisticated system balances the need for stable tooth positioning with the flexibility required for adaptive responses to functional demands and therapeutic interventions. From the microscopic arrangement of collagen fibres to the complex cellular signalling pathways that govern bone remodelling, every component works together to maintain optimal tooth position whilst permitting controlled movement when necessary. Understanding these mechanisms provides valuable insights into both normal oral physiology and the biological foundations of orthodontic treatment, helping explain why your teeth move slightly when pushed and how this movement can be harnessed therapeutically to achieve optimal dental alignment and function.